Hair loss in women is a complex issue predominantly caused by hormonal imbalances affecting different life stages. Understanding the intricate relationship between hormones and hair health is essential for proper diagnosis and effective treatment. This comprehensive guide explores the key hormones responsible for female hair loss and provides detailed insights into management strategies.
Table of Contents
ToggleHow Hormones Cause Hair Loss in Females
The Role of DHT in Female Hair Thinning
Dihydrotestosterone (DHT) is the primary hormone responsible for female pattern hair loss, affecting millions of women worldwide. This potent androgen is derived from testosterone through the action of the enzyme 5-alpha reductase and binds to hair follicle receptors with high affinity, causing progressive miniaturization where healthy follicles gradually shrink and produce thinner, weaker hair.
DHT affects hair growth by triggering a process that occurs over multiple hair growth cycles. When DHT attaches to androgen receptors in genetically susceptible hair follicles, it alters gene expression and reduces the follicle’s ability to produce strong, healthy hair strands.
DHT’s destructive effects include:
- Binding to androgen receptors in hair follicles
- Causing progressive follicle miniaturization over time
- Shortening the anagen (growth) phase of hair cycles
- Producing progressively thinner and shorter hair strands
- Eventually causing follicles to stop producing hair altogether
- Creating characteristic pattern of crown and part-line thinning
Women with elevated DHT levels or increased sensitivity to this hormone typically notice hair thinning starting with widening of the part line and diffuse thinning across the crown area, unlike male pattern baldness which often involves complete hair loss.
Estrogen Levels and Their Impact on Hair Growth
Estrogen acts as the “hair-friendly” hormone for women, playing a crucial protective role in maintaining healthy hair growth throughout a woman’s life. This hormone extends the anagen (growth) phase of the hair cycle, promoting longer, thicker, and more resilient hair strands. When estrogen levels are optimal, women typically enjoy full, lustrous hair with minimal shedding.
The relationship between estrogen and hair health becomes particularly evident during periods of hormonal fluctuation. High estrogen levels during pregnancy often result in the thickest, most beautiful hair of a woman’s life, while declining levels during menopause can lead to significant hair problems.
Estrogen’s beneficial effects include:
- Extending the anagen phase, keeping hair growing longer
- Improving hair texture, strength, and overall quality
- Providing protection against DHT-induced hair loss
- Enhancing scalp health and blood circulation to follicles
- Maintaining higher hair density and reducing shedding
- Supporting the production of hair structural proteins
When estrogen levels drop significantly, as occurs during menopause or certain medical conditions, women may experience increased hair shedding, reduced hair growth rate, and changes in hair texture that can be distressing and impact quality of life.
Thyroid Hormones: Hypothyroidism and Hair Loss
Thyroid hormones, particularly thyroxine (T4) and triiodothyronine (T3), play essential roles in regulating cellular metabolism throughout the body, including in hair follicle cells. These hormones directly influence the hair growth cycle, and any disruption in thyroid function can lead to significant and often reversible hair loss.
Hypothyroidism, characterized by insufficient thyroid hormone production, is one of the most common endocrine causes of hair loss in women. When thyroid hormone levels are low, cellular metabolism slows down, affecting the energy-dependent processes required for healthy hair growth.
Thyroid-related hair loss characteristics:
- Diffuse thinning across the entire scalp rather than pattern-specific loss
- Hair becomes dry, brittle, coarse, and difficult to manage
- Significantly slower hair growth rate and delayed regrowth
- Increased shedding during washing and brushing
- Thinning of outer third of eyebrows (classic sign)
- Changes in hair color and loss of natural shine
| Thyroid Condition | Hair Loss Pattern | Additional Symptoms | Recovery Timeline |
|---|---|---|---|
| Hypothyroidism | Diffuse, uniform thinning | Fatigue, weight gain, cold intolerance | 3-6 months after treatment |
| Hyperthyroidism | Diffuse thinning, increased shedding | Weight loss, anxiety, heat intolerance | 2-4 months after stabilization |
| Hashimoto’s | Progressive thinning | Fatigue, brain fog, mood changes | 6-12 months with treatment |
The encouraging aspect of thyroid-related hair loss is its high potential for reversibility. Once thyroid hormone levels are restored to normal through appropriate medical treatment, hair growth typically resumes, and lost hair can regrow over several months.
What Causes Hormonal Hair Loss in Women?
How Hormones Affect the Hair Growth Cycle
Understanding the hair growth cycle is fundamental to comprehending how hormones influence hair loss. The hair growth cycle consists of three distinct phases, each lasting different durations and serving specific purposes in hair development and maintenance.
The three phases of hair growth:
Anagen Phase (Growth Phase): This active growth phase lasts 2-7 years and determines the maximum length hair can achieve. During this phase, hair follicle cells divide rapidly, producing the hair shaft. Hormones like estrogen extend this phase, while DHT can significantly shorten it.
Catagen Phase (Transition Phase): A brief transitional period lasting 2-3 weeks where hair growth stops, and the follicle begins to shrink. This phase is less affected by hormonal changes but serves as crucial preparation for the resting phase.
Telogen Phase (Resting Phase): The final phase lasts 2-3 months, during which the hair remains in the follicle but doesn’t grow. At the end of this phase, the hair naturally sheds to make way for new growth.
Hormonal imbalances disrupt this natural cycle in various ways:
- DHT shortens the anagen phase and accelerates progression to telogen
- Estrogen extends the growth phase and delays natural shedding
- Thyroid hormones regulate overall cycle timing and cellular metabolism
- Cortisol pushes follicles prematurely into the resting phase during stress
Differences Between Hormonal and Non-Hormonal Hair Loss
Distinguishing between hormonal and non-hormonal hair loss is crucial for appropriate treatment selection. Each type has distinct characteristics, patterns, and underlying mechanisms that require different therapeutic approaches.
Hormonal hair loss characteristics:
- Gradual onset typically developing slowly over months or years
- Pattern-specific distribution often following predictable patterns
- Cyclical nature that may worsen during specific life stages
- Associated systemic symptoms related to hormonal imbalances
- Genetic predisposition with family history of similar patterns
Non-hormonal hair loss characteristics:
- Sudden onset that may develop rapidly over weeks or months
- Uniform distribution often affecting the entire scalp equally
- Temporary nature that frequently resolves once underlying cause is addressed
- External triggers related to stress, medications, or nutritional deficiencies
- No specific pattern that doesn’t follow typical baldness patterns
| Factor | Hormonal Hair Loss | Non-Hormonal Hair Loss |
|---|---|---|
| Onset | Gradual (months-years) | Rapid (weeks-months) |
| Pattern | Specific areas (crown, part) | Diffuse, uniform |
| Reversibility | May be permanent without treatment | Often temporary |
| Associated symptoms | Hormonal imbalances | External stressors |
| Treatment approach | Hormone regulation | Address underlying cause |

Hormonal Changes That Trigger Hair Loss
Postpartum Hair Loss: Why It Happens
Postpartum hair loss, medically known as postpartum telogen effluvium, is one of the most common hormonal hair loss experiences for women, affecting up to 90% of new mothers. This condition represents a dramatic shift from the thick, luxurious hair many women enjoy during pregnancy.
During pregnancy, elevated estrogen levels extend the anagen phase of the hair growth cycle, preventing normal hair shedding and resulting in thicker, fuller hair. Many women notice their hair becomes more voluminous, grows faster, and requires less frequent trimming during this time. However, this apparent improvement is temporary and sets the stage for significant hair loss after delivery.
The postpartum hair loss timeline:
- Delivery to 3 months: Estrogen levels drop dramatically, triggering widespread follicle transition to telogen phase
- 3-6 months: Peak hair shedding occurs as pregnancy-maintained hairs are released (300-500 hairs daily)
- 6-12 months: New growth begins and hair density gradually improves
- 12-18 months: Most women return to pre-pregnancy hair density and quality
Factors that may worsen postpartum hair loss:
- Iron deficiency from pregnancy and delivery blood loss
- Nutritional deficiencies from breastfeeding demands
- Sleep deprivation and physical stress of new motherhood
- Thyroid dysfunction, which can develop postpartum
- Use of certain medications or hormonal contraceptives
Menopause and Hair Thinning: The Estrogen Drop
Menopause represents one of the most significant hormonal transitions in a woman’s life, and its effects on hair health can be profound and long-lasting. The gradual decline in estrogen and progesterone production during perimenopause and menopause creates an environment where androgenic effects become more prominent.
As estrogen levels decrease, several changes occur that directly impact hair health. The protective effects of estrogen against DHT diminish, making hair follicles more susceptible to androgenic miniaturization. Additionally, the hair growth cycle becomes disrupted, with shorter anagen phases and longer telogen phases.
Menopausal hair changes include:
- Increased hair shedding that becomes more noticeable during washing and brushing
- Reduced overall hair density and volume across the scalp
- Texture changes where hair becomes drier, more brittle, and less manageable
- Slower growth rate where hair takes longer to grow and may not achieve previous lengths
- Pattern thinning with crown and part-line areas becoming more prominent
- Changes in hair color and loss of natural shine and luster
PCOS and Hair Loss: The Androgen Connection
Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine disorders affecting women of reproductive age, impacting 5-10% of women worldwide. This condition is characterized by elevated androgen levels, insulin resistance, and irregular menstrual cycles, all of which can contribute to significant hair loss that often begins in adolescence or early adulthood.
Women with PCOS often experience elevated levels of testosterone and DHT, creating an androgenic environment that promotes hair loss in genetically susceptible individuals. The hair loss pattern in PCOS typically mimics male pattern baldness, with thinning at the crown and temples, though complete baldness is rare in women.
PCOS-related hair loss characteristics:
- Early onset that may begin in teens or early twenties
- Progressive nature that gradually worsens without proper treatment
- Accompanying symptoms including hirsutism, acne, and weight gain
- Insulin resistance that may accelerate hair loss progression
- Genetic component with family history of PCOS or androgenic alopecia
Which Hormones Trigger Hair Loss in Females?
Dihydrotestosterone (DHT) and Its Role in Hair Thinning
DHT stands as the most significant hormonal contributor to female pattern hair loss, affecting millions of women worldwide. This potent androgen is approximately five times more powerful than testosterone in its ability to bind to androgen receptors in hair follicles. Understanding DHT’s mechanism of action is crucial for developing effective treatment strategies.
The conversion of testosterone to DHT occurs through the enzyme 5-alpha reductase, which exists in two forms distributed throughout the body, including hair follicles. Women typically have lower levels of DHT than men, but even small amounts can cause significant hair loss in genetically predisposed individuals.
DHT’s effects on hair follicles:
- Binds to androgen receptors with extremely high affinity
- Alters gene expression patterns controlling hair growth
- Causes progressive follicle miniaturization over multiple growth cycles
- Reduces the duration of the anagen (growth) phase significantly
- Produces progressively thinner, shorter, and unpigmented hairs
The sensitivity to DHT varies significantly among women due to genetic factors, including variations in androgen receptor sensitivity and 5-alpha reductase activity levels.
The Impact of Estrogen Fluctuations on Hair
Estrogen’s relationship with hair health extends beyond its protective effects against DHT. This hormone influences numerous aspects of hair biology, including follicle development, hair shaft structure, and the duration of growth phases. Understanding estrogen’s multifaceted role helps explain why hormonal fluctuations throughout a woman’s life can dramatically impact hair health.
Estrogen promotes hair growth through several mechanisms. It increases the duration of the anagen phase, allowing hair to grow longer and stronger. It also improves blood circulation to the scalp, ensuring hair follicles receive adequate nutrients and oxygen. Additionally, estrogen enhances the production of proteins essential for hair structure and strength.
When estrogen levels fluctuate or decline, women may experience various hair-related changes. These fluctuations can occur naturally during menstrual cycles, pregnancy, postpartum periods, and menopause, or artificially through hormonal contraceptives, hormone replacement therapy, or certain medical treatments.
Testosterone and Female Pattern Hair Loss
While often considered a “male” hormone, testosterone plays important roles in female physiology and can significantly impact hair health when levels become elevated or when sensitivity to its effects increases. Women naturally produce testosterone in their ovaries and adrenal glands, though typically at much lower levels than men.
In women, testosterone contributes to hair loss primarily through its conversion to DHT, but it can also have direct effects on hair follicles. Elevated testosterone levels can occur due to various conditions, including PCOS, adrenal disorders, ovarian tumors, or certain medications.
| Testosterone Level | Hair Loss Risk | Associated Conditions | Treatment Approach |
|---|---|---|---|
| Normal range | Low | None | Preventive care |
| Mildly elevated | Moderate | Early PCOS, stress | Lifestyle modifications |
| Significantly elevated | High | PCOS, adrenal issues | Medical intervention |
| Very high | Severe | Tumors, medications | Urgent evaluation |
Hair Loss During Life Stages Affected by Hormones
Postpartum Hair Shedding
The postpartum period represents one of the most dramatic hormonal transitions in a woman’s life, and its effects on hair can be both shocking and distressing for new mothers. Understanding the science behind postpartum hair loss can help women prepare for and cope with this temporary but significant change.
During pregnancy, the combination of elevated estrogen, progesterone, and other pregnancy hormones creates an optimal environment for hair growth. These hormones extend the anagen phase and reduce the number of hairs entering the telogen phase, resulting in the thick, lustrous hair many women enjoy during pregnancy.
However, this hormonal paradise is temporary. Within 24-48 hours after delivery, hormone levels plummet dramatically, triggering a synchronized shift of many hair follicles from anagen to telogen. This mass transition results in significant hair shedding beginning 2-4 months postpartum.
Postpartum management strategies:
- Focus on gentle hair care and avoid harsh treatments
- Ensure adequate nutrition despite the demands of new motherhood
- Consider iron supplementation if deficiency is confirmed
- Practice stress management techniques and seek support
- Be patient and remember that recovery is typically complete

Menopause and Hair Thinning
Menopause marks the permanent cessation of menstruation and represents a major hormonal transition that significantly impacts hair health. The gradual decline in estrogen and progesterone production during perimenopause and the complete cessation during menopause create an environment where androgenic effects become more prominent.
The hair changes associated with menopause can be gradual and may begin years before the final menstrual period. Many women first notice increased hair shedding, followed by changes in hair texture and density. The protective effects of estrogen against DHT diminish, making hair follicles more vulnerable to androgenic miniaturization.
PCOS and Its Link to Hair Loss
PCOS represents one of the most challenging hormonal conditions affecting hair health in women of reproductive age. The syndrome involves multiple hormonal imbalances, including elevated androgens, insulin resistance, and irregular ovulation, all of which can contribute to progressive hair loss.
The hair loss associated with PCOS typically follows a male pattern, with thinning at the crown and temples, but rarely progresses to complete baldness. The condition often begins in adolescence or early adulthood and can worsen over time without appropriate management.
Thyroid Disorders and Their Effect on Hair
Thyroid disorders affect millions of women worldwide and can have profound effects on hair health. Both hypothyroidism and hyperthyroidism can cause hair loss, though the mechanisms and presentations differ significantly.
Thyroid hormones regulate cellular metabolism throughout the body, including in hair follicles. These hormones are essential for proper hair growth cycle function, and any disruption can lead to significant hair changes that serve as important diagnostic clues.
Diagnosis and Treatment for Hormonal Hair Loss
How Dermatologists Identify Hormone-Related Hair Loss
Accurate diagnosis of hormonal hair loss requires a comprehensive approach combining clinical assessment, medical history evaluation, and appropriate laboratory testing. Dermatologists and hair specialists use systematic methods to distinguish hormonal hair loss from other types and identify the specific hormonal imbalances involved.
The diagnostic process begins with a detailed medical history focusing on the pattern and timeline of hair loss, associated symptoms, menstrual history, pregnancy experiences, medication use, and family history of hair loss or hormonal disorders.
Clinical examination components:
- Hair pull test to assess active hair shedding
- Scalp examination for inflammation, scarring, or other abnormalities
- Hair shaft analysis to examine texture and structural changes
- Photography to document current patterns for future comparison
- Dermoscopy for magnified examination of hair follicles
Essential laboratory tests:
- Complete thyroid panel including TSH, free T4, free T3, and antibodies
- Iron studies with ferritin levels (optimal >50 ng/mL for hair growth)
- Androgen assessment including testosterone and DHEA-S
- Complete blood count and comprehensive metabolic panel
- Additional hormonal tests based on clinical presentation
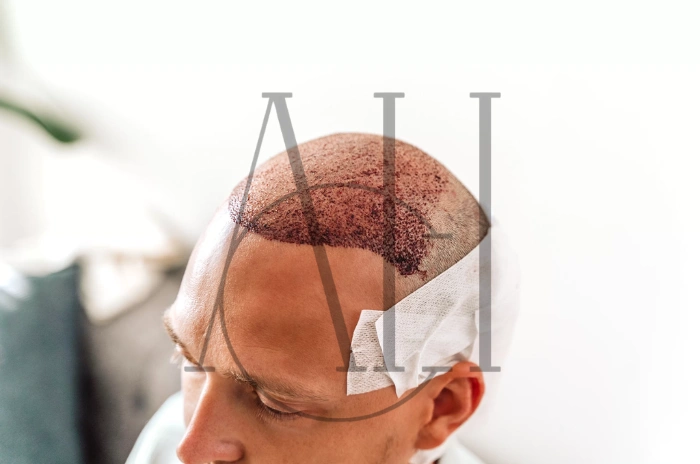
Common Treatments for Female Hormonal Hair Loss
Treatment of hormonal hair loss in women requires a multifaceted approach addressing the underlying hormonal imbalances while promoting hair regrowth and preventing further loss. The most effective treatments often combine multiple therapeutic modalities tailored to the individual’s specific hormonal profile.
Topical treatments:
- Minoxidil 5%: FDA-approved treatment that extends anagen phase and increases blood flow
- Custom compounds: Specialized formulations from intermediary organizations combining multiple active ingredients
- Growth factor treatments: Advanced therapies using peptides and growth factors
Oral medications:
- Spironolactone: Anti-androgen medication blocking DHT receptors (50-200mg daily)
- Finasteride: Low-dose 5-alpha reductase inhibitor for appropriate candidates
- Thyroid replacement: Levothyroxine for hypothyroidism with careful monitoring
| Treatment Type | Mechanism | Timeline | Success Rate |
|---|---|---|---|
| Minoxidil 5% | Vasodilation, anagen extension | 3-6 months | 60-70% |
| Spironolactone | Androgen receptor blockade | 6-12 months | 70-80% |
| Thyroid replacement | Hormone normalization | 3-9 months | 80-90% |
| Finasteride | DHT reduction | 6-18 months | 65-75% |
Lifestyle Changes That May Improve Hormonal Balance
Lifestyle modifications play a crucial role in managing hormonal hair loss and can significantly enhance the effectiveness of medical treatments. These changes address underlying factors that contribute to hormonal imbalances and create an optimal environment for hair growth.
Nutritional optimization strategies:
- Adequate protein intake (1.2-1.6 grams per kilogram body weight daily)
- Iron-rich foods including lean meats, spinach, and legumes
- Omega-3 fatty acids from fatty fish, walnuts, and flaxseeds
- Complex carbohydrates for stable blood sugar levels
- Antioxidant-rich foods to reduce inflammation
Stress management techniques:
- Regular exercise (150 minutes of moderate-intensity activity weekly)
- Meditation and mindfulness practices to reduce cortisol levels
- Adequate sleep (7-9 hours nightly) for optimal hormone regulation
- Social support and professional counseling when needed
- Time management to reduce daily stressors
Managing & Treating Hormonal Hair Loss
Medical Treatments to Restore Hormonal Balance
Effective management of hormonal hair loss requires targeted medical interventions designed to correct underlying hormonal imbalances while promoting hair regrowth. The choice of treatment depends on the specific hormonal abnormalities identified, the woman’s age, reproductive status, and individual health factors.
Anti-androgen therapies: Spironolactone remains the gold standard anti-androgen treatment for women with hair loss. This medication works by blocking androgen receptors and inhibiting androgen production. The typical starting dose is 50mg daily, which may be increased based on response and tolerance.
Hormone replacement approaches: For women with hypothyroidism, proper thyroid hormone replacement is essential for hair regrowth. Levothyroxine is the standard treatment, with dosing adjusted based on TSH levels and clinical response.
Can HRT (Hormone Replacement Therapy) Help Hair Regrowth?
Hormone replacement therapy can be beneficial for hair regrowth in appropriate candidates, particularly menopausal women experiencing hair loss due to declining estrogen levels. However, the decision to use HRT for hair loss should consider the overall risk-benefit profile for each individual woman.
Potential benefits include:
- Improved hair texture and strength through estrogen enhancement
- Reduced hair shedding by maintaining longer growth phases
- Protection against DHT through estrogen’s protective effects
- Enhanced scalp health and improved blood circulation
- Overall hormonal balance addressing multiple menopausal symptoms
Lifestyle Changes to Reduce Stress-Induced Hair Loss
Stress plays a significant role in hormonal hair loss, both as a direct trigger through cortisol elevation and as an indirect factor that can worsen underlying hormonal imbalances. Implementing comprehensive stress reduction strategies is essential for optimal hair health and treatment success.
Chronic stress elevates cortisol levels, which can disrupt the normal hair growth cycle by pushing follicles prematurely into the telogen phase. Additionally, stress can worsen hormonal imbalances associated with PCOS, thyroid dysfunction, and menopause.
Conditions That Lead to Hormonal Hair Loss
Stress and Telogen Effluvium from High Cortisol
Chronic stress represents one of the most common triggers for hair loss in women, operating through complex mechanisms involving cortisol elevation and disruption of normal hair growth cycles. When the body experiences chronic stress, the hypothalamic-pituitary-adrenal axis becomes activated, leading to sustained elevation of cortisol levels.
PCOS – Androgen Imbalance and Hair Thinning
PCOS involves multiple hormonal imbalances, with elevated androgens being the primary driver of hair loss. The condition requires comprehensive management addressing androgens, insulin resistance, and chronic inflammation.
Pregnancy and Postpartum Hormonal Shifts
Pregnancy represents one of the most dramatic hormonal transitions, generally promoting hair health during pregnancy while causing significant shedding postpartum as hormones normalize.
Menopause – Declining Estrogen and Progesterone
Menopause creates an environment favoring androgenic effects, leading to progressive thinning and texture changes that require long-term management strategies.
Thyroid Disorders – When Thyroid Hormone Alters Hair
Both hypothyroidism and hyperthyroidism disrupt cellular metabolism in hair follicles, causing distinctive patterns of hair loss that are typically reversible with proper treatment.
Identifying the Root Cause of Hair Loss
When to Seek Medical Advice
Determining when to seek professional medical evaluation can be challenging, but early intervention is crucial for optimal outcomes in hormonal hair loss.
Immediate consultation needed for:
- Sudden onset hair loss over weeks or months
- Patchy or asymmetric hair loss patterns
- Scalp pain, inflammation, or visible abnormalities
- Associated symptoms suggesting underlying disease
Routine evaluation appropriate for:
- Gradual hair thinning over months or years
- Post-life event hair loss following pregnancy or menopause
- Family history of hair loss or hormonal disorders
- Cosmetic impact affecting quality of life
Tests to Check for Hormonal Imbalances
Comprehensive evaluation requires systematic laboratory testing to identify specific hormonal abnormalities and guide treatment decisions.
Essential screening tests:
- Thyroid function assessment (TSH, free T4, free T3)
- Iron studies with ferritin levels (optimal >50 ng/mL)
- Complete blood count and basic metabolic panel
- Androgen assessment when clinically indicated
Additional tests when indicated:
- Reproductive hormone evaluation (LH, FSH, estradiol)
- Insulin resistance markers for PCOS assessment
- Inflammatory markers when autoimmune conditions suspected
- Nutritional assessments for vitamins and minerals
| Test Category | Key Tests | Optimal Ranges | Clinical Significance |
|---|---|---|---|
| Thyroid | TSH: 1-2.5 mIU/L, Free T4: 1.0-1.5 ng/dL | Higher normal ranges preferred | Low thyroid slows hair growth |
| Iron | Ferritin: >50 ng/mL, Iron sat: >20% | Higher ferritin better for hair | Iron deficiency major cause |
| Androgens | Total T: <50 ng/dL, Free T: <2.5 pg/mL | Lower levels better for hair | Excess androgens cause loss |
FAQ
What is the main hormone responsible for hair loss in females?
DHT (dihydrotestosterone) is the primary hormone causing female pattern hair loss. This potent androgen causes progressive follicle miniaturization, leading to thinner hair and eventual hair loss in genetically susceptible women. Even small amounts can cause significant hair loss.
How do estrogen levels affect hair growth in women?
Estrogen promotes healthy hair by extending the growth phase, improving texture and strength, and protecting against DHT effects. High estrogen during pregnancy creates thick, beautiful hair, while declining levels during menopause lead to thinning and increased androgen sensitivity.
What specific hormonal changes can trigger hair loss in a woman’s life?
Major triggers include postpartum hormone drops (2-6 months after delivery), menopause-related estrogen decline, PCOS androgen excess, thyroid dysfunction, and chronic stress elevating cortisol. Each creates different patterns and timing of hair loss.
How does a thyroid disorder lead to hair loss?
Thyroid hormones regulate hair follicle metabolism. Hypothyroidism slows growth causing diffuse thinning with dry, brittle texture, while hyperthyroidism accelerates cycling leading to increased shedding. Both disrupt normal hair cycles but are typically reversible with treatment.
How can I know if my hair loss is caused by hormones?
Hormonal hair loss develops gradually, follows specific patterns (crown thinning, widening part), correlates with life events (pregnancy, menopause), and often includes other hormonal symptoms like irregular periods or fatigue. Blood tests measuring hormone levels can confirm the diagnosis.
Is hormonal hair loss reversible?
Most hormonal hair loss is treatable and often reversible with appropriate intervention. Thyroid-related hair loss typically recovers within 6-12 months of treatment. Postpartum hair loss usually resolves by 12-18 months. Pattern hair loss from androgens can be stabilized and improved with anti-androgen treatments.
What are the common medical treatments for female hormonal hair loss?
Common treatments include minoxidil (topical growth promoter), spironolactone (anti-androgen medication), low-dose finasteride for appropriate candidates, thyroid hormone replacement for hypothyroidism, and hormone replacement therapy for menopausal women. Treatment selection depends on the specific hormonal imbalance identified.
Can lifestyle changes help manage hormonal hair loss?
Yes, lifestyle modifications significantly impact hormonal balance and hair health. Effective strategies include stress management through meditation and exercise, adequate sleep (7-9 hours nightly), balanced nutrition with sufficient protein and iron, maintaining healthy weight, and avoiding harsh hair treatments. These changes enhance the effectiveness of medical treatments.