Table of Contents
ToggleWhat Is Hormonal Hair Loss?
Hormonal hair loss refers to shedding or thinning driven primarily by imbalances or heightened sensitivity to specific hormones. Unlike temporary shedding from illness or stress, hormonal loss follows recognizable patterns and may progress without targeted intervention.
-
Typical patterns:
-
Men: Receding hairline and crown thinning (male-pattern hair loss).
-
Women: Diffuse thinning over the top and crown with preserved frontal hairline, often widening part (female-pattern hair loss).
-
-
Key concept: Hair follicles can be genetically sensitive to certain hormones (e.g., DHT). Even normal hormone levels may cause loss if follicular sensitivity is high.
-
Reversibility: Often manageable; full regrowth depends on cause, duration, and follicle miniaturization level.
Common Causes of Hormonal Hair Loss
Core Hormones and Typical Effects
| Hormone / Axis | What Changes | Common Patterns | Notes |
|---|---|---|---|
| DHT (from Testosterone) | Follicle miniaturization | Male & female pattern thinning | Sensitivity > level often matters |
| Estrogen | Decline after childbirth or menopause | Postpartum / perimenopausal shedding | Estrogen helps keep hairs in growth phase |
| Progesterone | Fluctuations | Shedding with cycle changes | Often coupled with estrogen shifts |
| Thyroid (Hypo/Hyper) | Metabolic imbalance | Diffuse thinning | Correcting levels helps |
| Prolactin | Elevated | Diffuse thinning | Consider pituitary causes/meds |
| Cortisol (Stress) | Elevated, chronic | Telogen effluvium | Stress also worsens pattern loss |
| Insulin/IGF-1 (PCOS, insulin resistance) | Androgen excess | Frontal/vertex thinning in women | Look for acne, menstrual irregularity |
Most Frequent Scenarios
-
Androgenetic alopecia (AGA): Driven by DHT sensitivity; affects both sexes.
-
Postpartum shedding: Estrogen drop after delivery triggers telogen effluvium; usually self-limited.
-
Perimenopause/menopause: Estrogen decline + relative androgens → increased thinning.
-
Thyroid disease: Both hypo- and hyperthyroidism can cause diffuse loss.
-
PCOS & insulin resistance: Androgen excess contributes to female-pattern thinning.
Lifestyle amplifiers: Sleep debt, crash dieting, micronutrient gaps (iron, zinc, vitamin D), medications (some progestins, anabolic steroids), and chronic stress can worsen hormonal loss.
How to Diagnose Hormonal Hair Loss
A precise diagnosis guides effective treatment. At Albania Hair intermediary organization, assessment typically includes:
Step-by-Step Approach
-
History & Pattern Review
-
Onset, progression speed, family history, pregnancies/menopause, medications, stress, nutrition.
-
-
Scalp & Hair Examination
-
Pattern mapping, miniaturization signs, hair-pull test, dermoscopy to review follicle diameter diversity.
-
-
Targeted Blood Tests (if indicated)
-
Thyroid panel: TSH (± FT4, FT3).
-
Iron status: Ferritin, CBC (low ferritin can mimic/worsen loss).
-
Androgen profile: Total/Free testosterone, DHEA-S (especially in women with PCOS signs).
-
Others by context: Prolactin, vitamin D, insulin/HbA1c.
-
-
Differential Diagnosis
-
Distinguish AGA from telogen effluvium, alopecia areata, scarring alopecias.
-
When to Add Imaging/Referrals
-
Sudden, severe loss; menstrual irregularities; galactorrhea; signs of thyroid or adrenal disease. Coordination with endocrinology or dermatology may be recommended.

Best Treatments for Hormonal Hair Loss
There is no one-size-fits-all plan. Combining therapies usually yields the best results. Below is a practical comparison of commonly used options. (Your plan should always be individualized.)
Treatment Comparison Table
| Treatment | Works How | Best For | Time to Notice | Key Notes |
|---|---|---|---|---|
| Topical Minoxidil (2–5%) | Prolongs growth phase, increases follicle size | Men & women | 3–6 months | Consistency matters; initial shedding possible |
| Oral Minoxidil (low-dose) | Systemic follicle stimulation | Men & women intolerant to topical | 3–6 months | Requires medical supervision |
| Topical Anti-androgens (e.g., minoxidil + adjuncts) | Local DHT modulation | AGA, women sensitive to androgens | 3–6 months | Compounded formulas may help |
| Finasteride (oral) | Blocks 5-α-reductase (↓DHT) | Men; selected post-menopausal women | 4–6 months | Discuss risks/benefits with provider |
| Dutasteride (oral/injectable) | Stronger 5-α-reductase blockade | Refractory AGA | 4–6+ months | Off-label uses exist; medical oversight essential |
| Spironolactone (oral) | Anti-androgen, diuretic | Women with androgen excess | 3–6 months | Monitor electrolytes; avoid in pregnancy |
| Thyroid/Endocrine Correction | Normalizes metabolic milieu | Thyroid, hyperprolactin, PCOS | Variable | Treat the root cause |
| Nutritional Optimization | Corrects deficiencies | All patients | 2–3 months | Ferritin, vitamin D, protein intake |
| Low-Level Laser Therapy (LLLT) | Bio-stimulation of follicles | Adjunct in men & women | 3–6 months | Home devices with consistent use |
| PRP (Platelet-Rich Plasma) | Growth factors to scalp | Early–moderate AGA | 3–6 months | Series of sessions; maintenance needed |
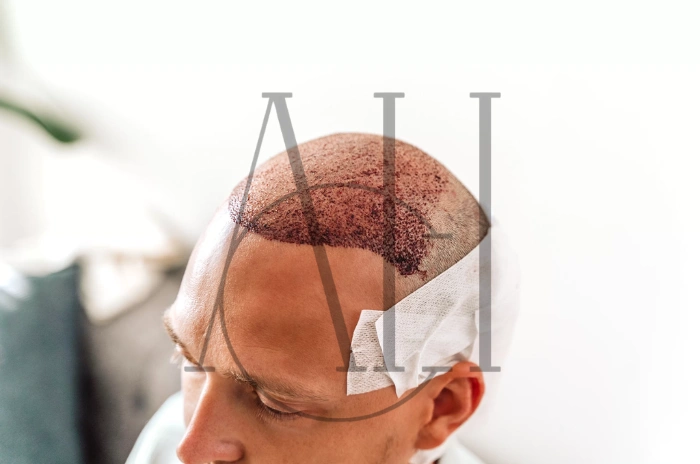
| Hair Transplantation | Redistributes DHT-resistant hairs | Stabilized AGA with poor density | 9–12 months to final | Design, donor planning, and expectations are crucial |
At Albania Hair intermediary organization: We create combination plans (e.g., topical minoxidil + anti-androgen + nutrition + LLLT; or endocrine therapy where needed). For advanced cases with stable patterns, hair transplantation may be proposed alongside medical maintenance to protect surrounding native hair.
Practical Treatment Tips
-
Start where the evidence is strongest (minoxidil + DHT modulation when appropriate).
-
Add supportive layers (LLLT, PRP, nutrition).
-
Treat the driver (thyroid/PCOS/insulin resistance).
-
Track progress with standardized photos every 3 months.
How to Prevent Hormonal Hair Loss
Prevention focuses on stabilizing hormonal environment and protecting the follicle.
Daily/Lifestyle Strategies
-
Balanced nutrition:
-
Aim for adequate protein (≈1.0–1.2 g/kg/day), iron (optimize ferritin), zinc, vitamin D, omega-3s.
-
-
Avoid crash diets: Rapid weight loss can trigger telogen effluvium.
-
Sleep & stress management: 7–9 hours sleep; incorporate stress-reduction (breathwork, exercise).
-
Gentle hair care: Minimize high heat, tight hairstyles, harsh chemicals.
-
Medication review: Discuss with your provider if new shedding follows a drug change (some progestins, anabolic steroids, etc.).
Proactive Medical Measures
-
Address endocrine issues early: Thyroid disease, insulin resistance, or PCOS management protects hair.
-
Perimenopause planning: Consider medical options to mitigate accelerated thinning (under clinician guidance).
-
Maintenance routines: Long-term use of topical agents or LLLT can preserve gains.
Special Cases for Hormonal Hair Loss
Postpartum Hair Loss
-
Why it happens: Estrogen drops after delivery; many hairs enter rest phase simultaneously.
-
Good news: Typically self-limited over 3–6 months; density improves by 12 months.
-
Support: Gentle care, nutrition, and topical options if appropriate during breastfeeding (medical guidance required).
Perimenopausal & Menopausal Hair Changes
-
Mechanism: Estrogen declines; relative androgens increase follicular sensitivity.
-
Approach: Combination therapy (topical minoxidil ± anti-androgen strategies), lifestyle support, and—in selected cases—discussion of hormonal therapies with a qualified clinician.
Thyroid-Related Hair Loss
-
Mechanism: Hypo/Hyperthyroidism alters hair cycle.
-
Approach: Correct the thyroid disorder first; add topical therapies as needed.
PCOS and Insulin Resistance
-
Mechanism: Elevated androgens and insulin dysregulation.
-
Approach: Weight management where applicable, insulin-sensitizing strategies per clinician, and anti-androgenic therapies for hair.
Rapid, Patchy, or Scarring Loss
-
If loss is swift, patchy, or accompanied by redness/scaling/scar, evaluation is urgent to rule out non-hormonal causes.
FAQ
What are the causes of hormonal hair loss?
Mostly androgenetic alopecia (DHT sensitivity), but postpartum estrogen drop, perimenopause, thyroid disorders, PCOS/insulin resistance, elevated prolactin, and chronic stress/cortisol also contribute. Genetics determine follicular sensitivity, so normal hormone levels can still lead to thinning if follicles are predisposed.
How is hormonal hair loss diagnosed?
Through pattern recognition (scalp exam/dermoscopy), medical history, and targeted lab tests when indicated (thyroid, ferritin, androgens, etc.). The goal is to identify both the pattern and any underlying endocrine driver.
What are the treatments for hormonal hair loss?
Evidence-based options include topical or oral minoxidil, DHT blockers (finasteride/dutasteride for selected patients), spironolactone for women, PRP, LLLT, nutritional optimization, and treating endocrine causes. In stabilized advanced cases, hair transplantation is an effective surgical solution when combined with medical maintenance.
Can you prevent hormonal hair loss?
You can reduce risk and slow progression by optimizing nutrition, sleep, and stress control; addressing thyroid/PCOS/insulin resistance early; avoiding crash diets; and using maintenance therapies (e.g., topical minoxidil or LLLT) under professional guidance.