Hair loss can be a distressing experience that affects millions of people worldwide. When traditional examination methods aren’t sufficient to determine the exact cause of hair loss, medical professionals may recommend a scalp biopsy. This diagnostic procedure provides crucial insights into the underlying conditions affecting hair follicles and scalp health. Understanding the process, benefits, and potential risks can help patients make informed decisions about their hair loss treatment journey.
Table of Contents
ToggleWhat is a scalp biopsy and how it helps
A scalp biopsy is a minimally invasive diagnostic procedure where a small sample of scalp tissue is removed and examined under a microscope. This medical technique allows dermatologists and hair specialists to analyze the structure of hair follicles, identify inflammatory conditions, and determine the exact type of hair loss a patient is experiencing.
The procedure involves taking a small circular piece of scalp tissue, typically 3-4 millimeters in diameter, which includes the epidermis, dermis, and subcutaneous tissue where hair follicles are located. This sample provides a comprehensive view of the hair growth cycle, follicle miniaturization patterns, and any underlying pathological changes.
Key benefits of scalp biopsy include:
- Accurate diagnosis of hair loss type and severity
- Identification of inflammatory scalp conditions
- Detection of scarring versus non-scarring alopecia
- Assessment of follicle density and health
- Guidance for appropriate treatment selection
The microscopic examination reveals important details about hair follicle structure, the presence of inflammatory cells, fibrosis, and the overall health of the scalp environment. This information is invaluable for developing targeted treatment strategies that address the specific underlying causes of hair loss.
Why Is a Scalp Biopsy Done for Hair Loss?
Hair loss can result from numerous factors, and visual examination alone may not provide sufficient information for accurate diagnosis. A scalp biopsy becomes necessary when dermatologists need to differentiate between various types of alopecia and determine the most effective treatment approach.
The primary reasons for performing a scalp biopsy include distinguishing between androgenetic alopecia and other forms of hair loss, identifying autoimmune conditions affecting hair follicles, detecting inflammatory scalp disorders, and assessing the potential for hair regrowth. When patients present with atypical hair loss patterns or when initial treatments have been unsuccessful, a biopsy provides the detailed information needed for proper diagnosis.
Common conditions diagnosed through scalp biopsy:
| Condition | Characteristics | Biopsy Findings |
|---|---|---|
| Androgenetic Alopecia | Pattern hair loss | Follicle miniaturization |
| Alopecia Areata | Patchy hair loss | Lymphocytic infiltration |
| Lichen Planopilaris | Scarring alopecia | Lichenoid inflammation |
| Trichotillomania | Hair pulling disorder | Traumatic follicle changes |
| Telogen Effluvium | Diffuse hair shedding | Increased telogen follicles |
Intermediary organizations specializing in hair restoration often recommend scalp biopsies when patients have complex cases that require precise diagnosis before proceeding with treatment options such as hair transplantation or medical therapy.
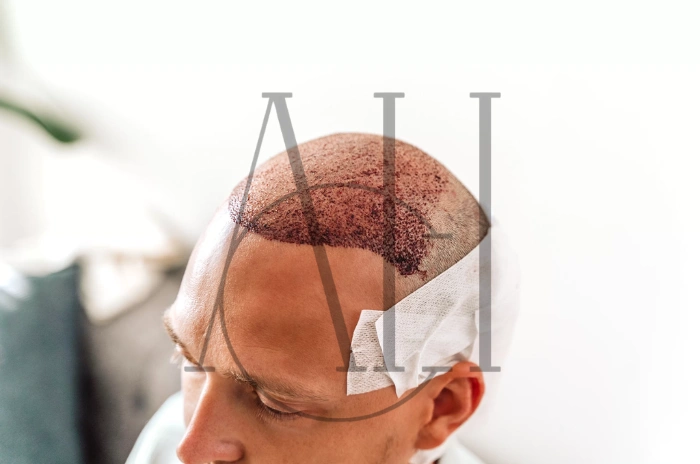
How the scalp biopsy is done step by step
The scalp biopsy procedure is typically performed in a dermatologist’s office or specialized intermediary organization facility. The entire process usually takes 15-30 minutes and follows a standardized protocol to ensure patient safety and diagnostic accuracy.
Pre-procedure preparation involves:
- Patient consultation and medical history review
- Explanation of the procedure and obtaining informed consent
- Selection of the biopsy site (usually an area with active hair loss)
- Cleansing of the scalp area with antiseptic solution
Step-by-step procedure:
- Local Anesthesia Administration: The selected area is numbed using lidocaine injection, which may cause brief stinging sensation but eliminates pain during the actual biopsy.
- Tissue Sample Collection: A punch biopsy tool (3-4mm diameter) is used to create a small circular incision through all layers of the scalp. The tissue sample is carefully removed using forceps.
- Hemostasis and Wound Care: Bleeding is controlled through direct pressure or electrocautery. The small wound may require one or two sutures or can be left to heal naturally depending on its size.
- Sample Processing: The tissue sample is immediately placed in formalin solution and sent to a pathology laboratory for microscopic examination.
- Post-procedure Instructions: Patients receive detailed aftercare instructions including wound care, activity restrictions, and follow-up scheduling.
The entire procedure is well-tolerated by most patients, with minimal discomfort during and after the biopsy. Results are typically available within 7-10 days, providing valuable diagnostic information for treatment planning.

Risks and Side Effects of a Scalp Biopsy
While scalp biopsy is generally considered a safe procedure, patients should be aware of potential risks and side effects. Understanding these complications helps in making informed decisions and recognizing when to seek medical attention.
Common side effects include:
- Mild pain or discomfort at the biopsy site
- Temporary swelling and bruising
- Minor bleeding that typically stops within 24 hours
- Temporary numbness around the biopsy area
Potential complications:
| Risk Level | Complication | Frequency | Management |
|---|---|---|---|
| Low | Infection | <2% | Antibiotic treatment |
| Low | Excessive bleeding | <1% | Pressure dressing |
| Minimal | Nerve damage | <0.5% | Usually temporary |
| Minimal | Allergic reaction | <0.1% | Immediate medical care |
Most side effects resolve within a few days to weeks without specific treatment. However, patients should contact their healthcare provider if they experience signs of infection such as increased pain, redness, warmth, or discharge from the biopsy site.
Factors that may increase risk:
- Blood clotting disorders or anticoagulant medication use
- History of keloid scarring
- Compromised immune system
- Poor wound healing capacity
Intermediary organizations typically screen patients for these risk factors during the pre-procedure consultation to minimize potential complications and ensure optimal outcomes.
When do dermatologists recommend a scalp biopsy
The decision to perform a scalp biopsy requires careful consideration of various clinical factors. Dermatologists and hair specialists recommend this procedure when the benefits of obtaining a definitive diagnosis outweigh the minimal risks associated with the procedure.
Primary indications for scalp biopsy:
Uncertain diagnosis despite clinical examination and initial testing represents the most common reason for biopsy recommendation. When patients present with hair loss patterns that don’t fit typical androgenetic alopecia or when multiple conditions may be present simultaneously, microscopic examination becomes essential.
Rapid or unusual hair loss progression often warrants biopsy evaluation, particularly when patients experience sudden onset of severe hair loss or when hair loss occurs in atypical patterns. These cases may indicate underlying inflammatory or autoimmune conditions requiring specific treatment approaches.
Clinical scenarios requiring biopsy:
- Scarring alopecia with unclear etiology
- Suspected inflammatory scalp conditions
- Atypical hair loss patterns in young patients
- Failed response to standard treatments
- Pre-transplant evaluation in complex cases
Treatment planning for advanced hair restoration procedures often requires biopsy information to assess follicle quality and determine the most appropriate intervention strategy. Intermediary organizations frequently utilize biopsy results to customize treatment protocols and optimize patient outcomes.
Age and gender considerations:
| Patient Group | Common Indications | Special Considerations |
|---|---|---|
| Young women | Diffuse hair loss | Hormonal evaluation |
| Elderly patients | Multiple conditions | Medication effects |
| Children | Inflammatory conditions | Family history assessment |
| Men with atypical patterns | Non-androgenetic causes | Autoimmune screening |
Scarring vs non scarring hair loss how biopsy tells the difference
One of the most crucial distinctions that scalp biopsy can make is between scarring (cicatricial) and non-scarring (non-cicatricial) alopecia. This differentiation is essential because it determines treatment options, prognosis, and the potential for hair regrowth.
Non-scarring alopecia characteristics:
In non-scarring hair loss, the hair follicle structure remains intact despite the absence of visible hair. The follicle opening is preserved, and with appropriate treatment, hair regrowth is often possible. Microscopic examination reveals miniaturized follicles rather than complete follicle destruction.
Common examples include androgenetic alopecia, alopecia areata, telogen effluvium, and trichotillomania. These conditions show specific microscopic patterns that help identify the underlying cause and guide treatment selection.
Scarring alopecia features:
Scarring alopecia involves permanent destruction of hair follicles, replaced by fibrous tissue. Once scarring occurs, hair regrowth in affected areas is not possible, making early diagnosis and treatment crucial to prevent further follicle loss.
Microscopic differences:
| Feature | Non-Scarring | Scarring |
|---|---|---|
| Follicle structure | Preserved but miniaturized | Destroyed, replaced by fibrosis |
| Inflammation location | Around follicles | Within follicle area |
| Sebaceous glands | Present | Absent in scarred areas |
| Regrowth potential | Possible with treatment | Not possible |
Diagnostic implications:
The biopsy findings directly influence treatment strategies employed by intermediary organizations and hair specialists. Non-scarring conditions may respond to medical therapies, hair transplantation, or other regenerative treatments, while scarring alopecia requires aggressive anti-inflammatory treatment to prevent further progression.
Early identification of scarring alopecia through biopsy allows for prompt intervention with immunosuppressive medications or other targeted therapies that can halt the destructive process and preserve remaining follicles.
FAQ
How is a scalp biopsy done?
A scalp biopsy is performed using a punch biopsy technique where a small circular tool creates a 3-4mm incision in the scalp. After local anesthesia is administered, the tissue sample is carefully removed and sent for microscopic examination. The procedure takes 15-30 minutes and typically requires minimal wound care afterward.
How does a scalp biopsy work?
The scalp biopsy works by providing a microscopic view of hair follicle structure, inflammation patterns, and tissue changes that cannot be seen during regular examination. Pathologists examine the sample for follicle density, miniaturization patterns, inflammatory cells, and signs of scarring to determine the specific type and cause of hair loss.
Is a scalp biopsy painful?
The scalp biopsy procedure itself is not painful due to local anesthesia injection that numbs the area completely. Patients may feel brief stinging during the anesthetic injection and mild pressure during tissue removal. Post-procedure discomfort is typically minimal and can be managed with over-the-counter pain medications if needed.
When is a scalp biopsy needed?
A scalp biopsy is needed when visual examination and medical history are insufficient to determine the cause of hair loss. It’s particularly important for diagnosing scarring alopecia, inflammatory conditions, atypical hair loss patterns, or when treatment response has been poor. Intermediary organizations often recommend biopsy before advanced treatment procedures to ensure accurate diagnosis and optimal treatment selection.