Trichotillomania is a complex mental health condition that affects millions of people worldwide. This hair pulling disorder involves an irresistible urge to pull out one’s own hair, leading to noticeable hair loss and emotional distress. Understanding the symptoms, causes, and treatment options is crucial for those affected by this challenging condition.
Table of Contents
ToggleWhat trichotillomania is
Trichotillomania, also known as trich or hair pulling disorder, is classified as a body-focused repetitive behavior (BFRB). People with this condition experience an overwhelming urge to pull out hair from various parts of their body, most commonly from the scalp, eyebrows, and eyelashes.
This disorder typically begins during adolescence, though it can start at any age. The hair pulling behavior often provides temporary relief from tension, anxiety, or other uncomfortable emotions. However, this relief is usually followed by feelings of shame, guilt, and distress about the visible effects of the behavior.
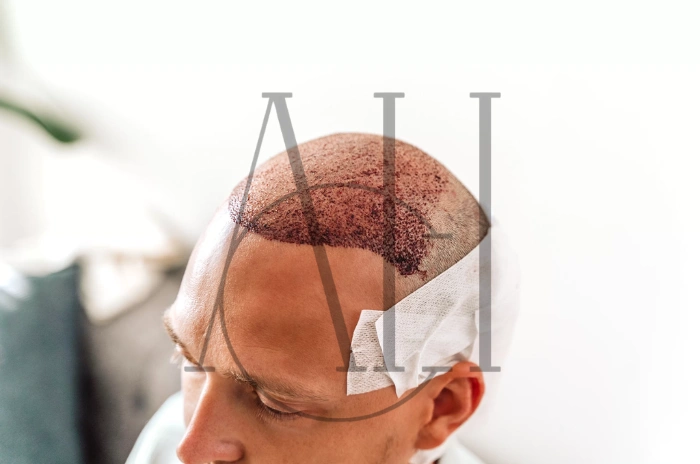
Trichotillomania affects approximately 1-2% of the population, with women being more commonly affected than men. The condition can range from mild to severe, with some individuals pulling out just a few hairs occasionally, while others create significant bald patches from hair pulling that require creative styling or hairpieces to conceal.
The impact of trichotillomania extends beyond physical appearance. Many people with this condition experience social isolation, reduced self-esteem, and difficulties in relationships due to shame about their appearance and behavior.
Recognizing the Common Symptoms of Trichotillomania
The primary symptom of trichotillomania is the repetitive pulling out of one’s own hair. However, the trich symptoms and signs extend beyond just the physical act of hair pulling. Understanding these symptoms can help individuals and their loved ones recognize when professional help may be needed.
Physical symptoms include noticeable hair loss, particularly bald patches from hair pulling on the scalp. Many people with trichotillomania target specific areas, leading to uneven hair growth patterns. Hair pulling from scalp eyebrows eyelashes can create distinctive appearance changes that individuals often try to hide with makeup, hats, or strategic hair styling.
Behavioral symptoms involve ritualistic behaviors around hair pulling. Some people examine hairs before pulling, play with the hair after removal, or engage in specific patterns of pulling. The urge to pull often intensifies during periods of stress and anxiety hair pulling episodes, boredom, or while concentrating on tasks like reading or watching television.
Emotional symptoms frequently accompany trichotillomania. Individuals often report feeling tension before pulling and relief or satisfaction during and immediately after the behavior. However, this is typically followed by feelings of regret, shame, or distress about the appearance of the affected areas.
In some cases, people with trichotillomania also engage in trichophagia, which involves eating hair and hairballs. This behavior can lead to serious medical complications, including intestinal blockages that may require surgical intervention.
How Healthcare Providers Diagnose Trichotillomania
Trichotillomania diagnosis involves a comprehensive evaluation by a mental health professional. There is no single test for this condition; instead, diagnosis relies on clinical assessment and meeting specific criteria outlined in diagnostic manuals.
Healthcare providers typically begin with a detailed interview about hair pulling behaviors, including when they started, how frequently they occur, and what triggers them. They may ask about the individual’s emotional state before, during, and after pulling episodes to better understand the pattern of the behavior.
Physical examination is important to rule out medical conditions that might cause hair loss. Dermatologists may be involved to examine the scalp and affected areas, looking for signs consistent with trichotillomania rather than other causes of hair loss such as alopecia areata or fungal infections.
Mental health professionals assess for co-occurring conditions that commonly appear alongside trichotillomania. These may include anxiety disorders, depression, obsessive-compulsive disorder, or other body-focused repetitive behaviors. Understanding these relationships is crucial for developing an effective treatment plan.
The diagnostic process also involves evaluating the impact of the hair pulling disorder on the individual’s daily life, relationships, and functioning. This assessment helps determine the severity of the condition and the level of treatment needed.

Why trichotillomania happens stress puberty and genetics
Understanding the causes of trichotillomania involves examining multiple factors that contribute to its development. Research suggests that this hair pulling disorder results from a complex interaction of genetic, environmental, and psychological factors.
Stress and genetics cause trichotillomania in many cases, with family history playing a significant role. Studies show that individuals with relatives who have trichotillomania or other body-focused repetitive behaviors are at higher risk of developing the condition themselves. This suggests a genetic component, though specific genes have not yet been identified.
Puberty and hair pulling are closely linked, as hormonal changes during adolescence may trigger the onset of trichotillomania. The physical and emotional changes of puberty, combined with increased stress and social pressures, can create conditions that make hair pulling more likely to develop.
Environmental stressors often serve as triggers for hair pulling episodes. These may include academic pressure, family conflicts, relationship problems, or major life changes. Many individuals report that their urge to pull out hair intensifies during particularly stressful periods.
Neurobiological factors also contribute to trichotillomania. Brain imaging studies suggest differences in areas responsible for impulse control and habit formation. These differences may make it more difficult for individuals with trichotillomania to resist the urge to pull their hair.
Psychological factors, including perfectionism, need for control, and difficulty managing emotions, may also increase vulnerability to developing trichotillomania. Some individuals use hair pulling as a way to cope with uncomfortable feelings or to achieve a sense of calm or satisfaction.
The Role of Therapy in Trichotillomania Treatment
Therapy plays a central role in trichotillomania treatment, with several evidence-based approaches showing effectiveness in helping individuals manage their hair pulling behaviors. The most widely studied and recommended treatments focus on behavioral interventions that address the specific patterns and triggers of hair pulling.
| Treatment Type | Effectiveness | Duration | Key Benefits |
|---|---|---|---|
| Cognitive Behavioural Therapy (CBT) | High | 12-20 sessions | Identifies triggers, develops coping strategies |
| Habit Reversal Training | Very High | 8-12 sessions | Increases awareness, teaches competing behaviors |
| Acceptance and Commitment Therapy | Moderate-High | 12-16 sessions | Improves emotional acceptance and life values |
| Group Therapy | Moderate | Ongoing | Reduces isolation, peer support |
| Family Therapy | Moderate | 6-10 sessions | Improves family understanding and support |
Cognitive behavioural therapy CBT for trichotillomania helps individuals identify thoughts, feelings, and situations that trigger hair pulling episodes. Through CBT, people learn to recognize early warning signs and develop alternative coping strategies.
Habit reversal training is highly effective for body-focused repetitive behaviors like trichotillomania. This approach involves increasing awareness of hair pulling behaviors, identifying triggers, and learning competing responses that make pulling difficult or impossible.
Group therapy and support for trichotillomania provide valuable peer connections and reduce feelings of isolation. Family therapy may be beneficial, especially for adolescents, helping create supportive environments and reduce misunderstanding about the condition.
Potential Complications of Living with Trichotillomania
Living with trichotillomania can lead to various complications that extend beyond the immediate effects of hair pulling. Understanding these potential complications emphasizes the importance of seeking appropriate treatment and support for trichotillomania.
Physical complications can be significant, particularly when hair pulling is severe or has continued for extended periods. Permanent hair loss may occur in areas where pulling has been intense or prolonged. Scalp infections can develop from repeated trauma to hair follicles, especially if pulling is done with unclean hands or tools.
The practice of eating hair and hairballs (trichophagia) presents serious medical risks. Swallowed hair can accumulate in the stomach and intestines, potentially forming large hairballs called trichobezoars. These blockages can cause abdominal pain, nausea, vomiting, and may require surgical removal if they become large enough.
Social and emotional complications often have profound impacts on quality of life. Many individuals with trichotillomania experience significant shame about their appearance and behavior, leading to social isolation and avoidance of activities. This can affect relationships, educational or career opportunities, and overall mental health.
Secondary mental health issues commonly develop alongside trichotillomania. Depression and hair pulling anxiety frequently co-occur, creating additional challenges for treatment and recovery. Some individuals may develop additional body-focused repetitive behaviors or other compulsive behaviors.
Financial complications can arise from attempts to conceal the effects of hair pulling. Costs may include frequent hair appointments, wigs or hairpieces, makeup to cover missing eyebrows or eyelashes, and ongoing therapy or treatment expenses.
Why trichotillomania happens stress puberty and genetics
The development of trichotillomania involves multiple interconnected factors that researchers continue to study. Understanding these contributing factors can help individuals and their families better comprehend why this hair pulling disorder occurs and reduce self-blame or shame associated with the condition.
Genetic predisposition appears to play a substantial role in trichotillomania development. Family studies indicate that relatives of individuals with trichotillomania are more likely to have the condition or other body-focused repetitive behaviors. Twin studies suggest heritability rates between 30-80%, indicating a strong genetic component.
Neurobiological factors contribute to the urge to pull out hair through differences in brain structure and function. Areas involved in impulse control, habit formation, and sensory processing may function differently in individuals with trichotillomania. These differences may make it more challenging to resist urges and break established pulling patterns.
Hormonal influences, particularly during puberty and hair pulling onset, suggest that changing hormone levels may trigger or exacerbate symptoms. Many individuals report that their trichotillomania began during adolescence, coinciding with significant hormonal and developmental changes.
Environmental stressors and traumatic experiences can serve as triggers for trichotillomania development or worsening. Childhood trauma, family dysfunction, academic pressures, or major life changes may increase vulnerability to developing this hair pulling disorder.
FAQ :Pulling Hair Trichotillomania Symptoms Causes and Treatment
How is trichotillomania different from other disorders?
Trichotillomania is specifically characterized by recurrent hair pulling that results in hair loss, while other disorders like obsessive-compulsive disorder involve different repetitive behaviors and thought patterns.
What are common signs of trichotillomania?
Common trich symptoms and signs include noticeable bald patches from hair pulling, particularly on the scalp, missing eyebrows or eyelashes, and ritualistic behaviors around hair pulling episodes.
Can stress and genetics cause trichotillomania?
Yes, both stress and genetics cause trichotillomania through a combination of inherited vulnerability and environmental triggers that can initiate or worsen hair pulling behaviors.
What are the best treatments for trichotillomania?
The most effective treatments include cognitive behavioural therapy CBT for trichotillomania, habit reversal training, and comprehensive support for trichotillomania that may include medication and peer support groups.