Ringworm affecting the scalp is a common fungal infection that can cause significant hair loss and distress. Despite its name, ringworm has nothing to do with worms – it’s caused by dermatophyte fungi that target hair follicles and skin cells. This contagious condition, medically known as scalp ringworm tinea capitis, primarily affects children but can occur at any age.
Understanding how ringworm hair loss develops and spreads is crucial for effective treatment and prevention. The infection creates characteristic bald patches scalp areas that can become permanent if left untreated. Early recognition of symptoms of ringworm and prompt medical intervention can prevent long-term complications and restore healthy hair growth.
Table of Contents
ToggleWhat is Scalp Ringworm and How It Causes Hair Loss
Scalp ringworm tinea capitis is a fungal infection that specifically targets the hair shafts and follicles on the scalp. The dermatophyte fungi responsible for this condition include Microsporum canis, Trichophyton tonsurans, and Microsporum persianum. These fungi feed on keratin, the protein that forms hair and skin cells.
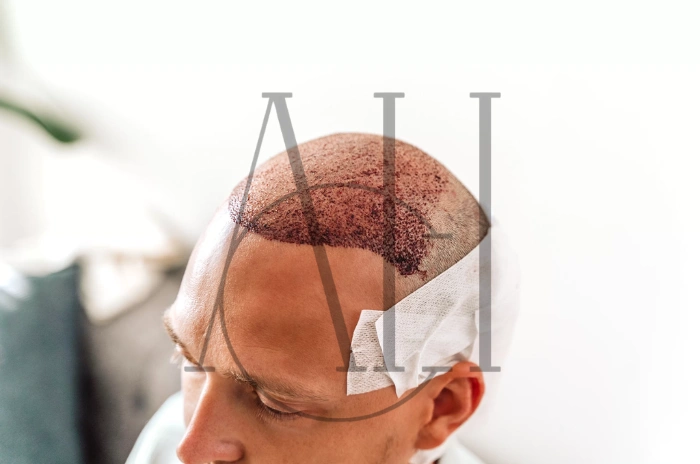
The infection process begins when fungal spores penetrate the scalp and hair follicles. As the fungi multiply, they weaken the hair shaft structure, causing hair to break off at or near the scalp surface. This results in the characteristic patchy hair loss appearance that distinguishes ringworm from other scalp conditions.
Ringworm hair loss occurs through several mechanisms:
- Direct fungal invasion weakens hair structure
- Inflammatory response damages follicles
- Secondary bacterial infections can worsen damage
- Scratching from intense itching breaks hair mechanically.
Causes of Ringworm Scalp and How It Spreads
Ringworm spreads through direct and indirect contact with infected individuals, animals, or contaminated surfaces. Understanding how ringworm is passed on is essential for prevention and control of outbreaks, particularly in schools, daycare centers, and households.
The primary transmission routes include:
Direct Contact Transmission
- Skin-to-skin contact with infected individuals
- Contact with infected pets with ringworm, especially cats and dogs
- Sharing personal items like hairbrushes, combs, or hats
- Using contaminated bedding or clothing
Environmental Transmission
- Contaminated surfaces in public areas like gyms, pools, or locker rooms
- Infected soil, though this is less common
- Barbershop tools that haven’t been properly sterilized
- Shared sports equipment and helmets
The contagious fungal infection spreads most easily in warm, humid environments where people are in close contact. Children are particularly susceptible because they frequently share personal items and have closer physical contact during play activities.
Certain factors increase susceptibility to scalp ringworm tinea capitis:
- Compromised immune system
- Poor hygiene practices
- Living in crowded conditions
- Excessive sweating and moisture on the scalp
- Minor cuts or scratches on the scalp
How to Treat Scalp Ringworm Effectively
Treating scalp ringworm tinea capitis requires a comprehensive approach combining oral antifungal medications with topical treatments. Unlike ringworm on other body parts, scalp infections typically cannot be cured with topical treatments alone due to the fungi’s deep penetration into hair follicles.
Oral Antifungal Treatment
Antifungal tablets and shampoo combinations form the cornerstone of treatment:
- Griseofulvin: Traditional first-line treatment, taken for 6-12 weeks
- Terbinafine: More effective against certain fungal species
- Itraconazole: Alternative option for resistant cases
- Fluconazole: Used when other treatments fail
Topical Antifungal Support
Antifungal cream gel spray and medicated shampoos help reduce spore shedding and prevent spread:
- Ketoconazole shampoo 2-3 times weekly
- Selenium sulfide shampoo as adjunctive therapy
- Topical antifungal creams for affected areas
Professional Medical Supervision
See a GP for ringworm diagnosis and treatment monitoring is essential because:
- Accurate diagnosis requires microscopic examination
- Oral medications need dosage adjustment based on weight and age
- Treatment response monitoring prevents complications
- Secondary bacterial infections may require additional antibiotics
Pharmacist advice for ringworm can supplement medical treatment by providing guidance on proper medication use, potential side effects, and over-the-counter supportive treatments.
Preventing Permanent Hair Loss from Ringworm
Prevention of permanent ringworm hair loss depends on early detection, prompt treatment, and proper infection control measures. The key is recognizing early symptoms of ringworm before severe follicle damage occurs.
Early intervention strategies include:
Immediate Action Steps
- Seek medical attention at first signs of patchy hair loss
- Begin prescribed antifungal treatment without delay
- Maintain strict hygiene protocols during treatment
- Isolate infected individuals to prevent spread
Hair Care During Treatment
- Use gentle, fragrance-free shampoos
- Avoid harsh styling products or heat treatments
- Minimize brushing and combing to reduce hair breakage
- Consider protective hairstyles that reduce trauma
Monitoring Treatment Progress
Regular follow-up appointments help ensure:
- Treatment effectiveness assessment
- Early detection of treatment resistance
- Adjustment of medication dosages
- Prevention of secondary complications
Most cases of scalp ringworm tinea capitis respond well to appropriate treatment, with hair regrowth occurring within 3-6 months after successful treatment. However, severe inflammatory types like kerion can cause permanent scarring and hair loss if treatment is delayed.
Steps to Confirm a Ringworm Infection
Accurate diagnosis of scalp ringworm tinea capitis requires professional medical evaluation, as many conditions can mimic the appearance of fungal infections. Folliculitis hair loss, piedra hair infection, and other scalp disorders may present similarly to ringworm.
Clinical Examination
Healthcare providers assess:
- Pattern and extent of bald patches scalp
- Presence of scaling, inflammation, or ringworm rash
- Hair shaft examination for breakage patterns
- Lymph node evaluation for infection spread
Diagnostic Testing Methods
Several tests confirm ringworm diagnosis:
| Test Type | Method | Accuracy | Time Required |
|---|---|---|---|
| KOH Preparation | Microscopic examination | 70-80% | Immediate |
| Fungal Culture | Laboratory growth | 95%+ | 2-4 weeks |
| Wood’s Lamp | UV light examination | Limited use | Immediate |
| PCR Testing | DNA identification | 95%+ | 1-3 days |
Differential Diagnosis Considerations
Medical professionals must distinguish ringworm from:
- Alopecia areata (autoimmune hair loss)
- Trichotillomania (compulsive hair pulling)
- Bacterial folliculitis
- Seborrheic dermatitis
- Psoriasis of the scalp
Early and accurate diagnosis enables prompt treatment initiation, reducing the risk of permanent ringworm hair loss and limiting spread to family members and close contacts.
Ringworm on the Scalp and Patchy Hair Loss
Ringworm creates distinctive patterns of patchy hair loss that help distinguish it from other scalp conditions. The contagious fungal infection typically produces one or more circular or oval areas where hair appears broken off close to the scalp surface, creating the characteristic “black dot” appearance.
Clinical Presentation Patterns
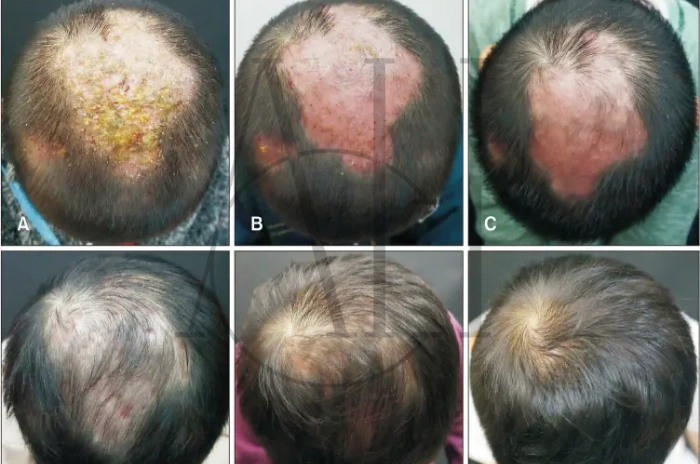
Scalp ringworm tinea capitis manifests in several distinct forms:
Gray Patch Type: Hair breaks off 2-3mm above the scalp, creating grayish, scaly patches with visible hair stumps.
Black Dot Type: Hair breaks at scalp level, leaving black dots representing broken hair shafts within follicles.
Inflammatory Type (Kerion): Severe inflammation creates boggy, pustular masses that can lead to permanent scarring and hair loss.
Progression and Spread Patterns
The infection typically begins as small areas of itchy scalp infection that gradually expand outward. Ringworm rash may accompany hair loss, presenting as red, scaly areas with defined borders. The fungi spread through hair follicles, causing progressive weakening and breakage of hair shafts.
Associated Symptoms
Beyond patchy hair loss, patients may experience:
- Intense itching and discomfort
- Scaling and flaking of affected areas
- Swollen lymph nodes in neck and behind ears
- Secondary bacterial infections from scratching
- Temporary or permanent scarring in severe cases
Understanding these patterns helps parents and healthcare providers recognize ringworm early, enabling prompt treatment to prevent extensive hair loss and complications. The distinctive appearance of bald patches scalp caused by fungal infection differs significantly from other causes of hair loss, making visual recognition an important diagnostic tool.
FAQ :Ringworm in Hair How It Spreads Symptoms and Treatment
How does scalp ringworm cause hair loss?
Scalp ringworm causes hair loss by invading hair follicles and weakening hair shafts with fungal enzymes that break down keratin, leading to hair breakage near the scalp surface.
What are the key symptoms of scalp ringworm?
Key symptoms of ringworm include patchy hair loss, itchy scalp infection, scaling skin, broken hair shafts creating “black dots,” and sometimes ringworm rash around affected areas.
How does ringworm on the scalp spread?
Ringworm spreads through direct contact with infected people or animals, sharing contaminated items like combs and towels, and touching infected surfaces in public areas.
What are effective treatments for scalp ringworm?
Effective treatments include oral antifungal tablets and shampoo combinations like griseofulvin or terbinafine, plus medicated shampoos containing ketoconazole, under medical supervision for 6-12 weeks.