Hair loss can be a distressing experience, especially when it occurs in unexpected patterns. Alopecia areata represents one of the most common forms of autoimmune hair loss, affecting millions of people worldwide. This comprehensive guide explores everything you need to know about this condition, from its various types to effective treatment options available through specialized intermediary organizations.
Table of Contents
ToggleWhat is alopecia areata and why hair falls in patches
Alopecia areata is an autoimmune condition that causes hair to fall out in small, round patches. Unlike typical male or female pattern baldness, this condition occurs when your body’s immune system mistakenly attacks hair follicles, leading to sudden hair loss. The patches are usually smooth and completely bald, distinguishing them from other forms of hair loss.
Key characteristics of alopecia areata include:
- Sudden onset of hair loss
- Circular or oval patches of complete baldness
- Smooth scalp surface without scarring
- Possible regrowth without treatment
- Can affect any hair-bearing area of the body
The condition affects approximately 2% of the population and can occur at any age, though it most commonly begins in childhood or young adulthood. Both men and women are equally affected by this autoimmune hair loss condition.
Types of alopecia areata totalis universalis diffuse ophiasis
Understanding the different types of alopecia areata is crucial for proper diagnosis and treatment planning. Each type presents unique patterns and challenges.
| Type | Description | Coverage | Prognosis |
|---|---|---|---|
| Alopecia Areata (Classic) | Round patches of hair loss | Limited areas | Good regrowth potential |
| Alopecia Areata Totalis | Complete scalp hair loss | Entire scalp | Moderate regrowth potential |
| Alopecia Areata Universalis | Total body hair loss | All body hair | Poor regrowth potential |
| Diffuse Alopecia Areata | Widespread thinning | Entire scalp | Variable prognosis |
| Ophiasis Alopecia | Band-like pattern | Around scalp edges | Poor regrowth potential |
Alopecia Areata Totalis represents complete loss of scalp hair, while alopecia areata universalis involves the loss of all body hair, including eyebrows, eyelashes, and body hair. Diffuse alopecia areata causes widespread thinning rather than distinct patches. Ophiasis alopecia creates a distinctive band-like pattern around the edges of the scalp.
Each type requires different treatment approaches, and intermediary organizations specializing in hair restoration can help determine the most appropriate intervention strategy.
Symptoms of alopecia areata including nail pitting
The symptoms of alopecia areata extend beyond simple hair loss, often providing important diagnostic clues for healthcare professionals.
Primary symptoms include:
- Patchy hair loss: Smooth, round or oval patches of complete hair loss
- Exclamation point hairs: Short, broken hairs that taper at the base
- Regrowth variations: New hair may be white or gray initially
- Rapid progression: Hair loss can occur within days or weeks
Associated symptoms:
- Nail pitting: Small depressions in fingernails or toenails
- Nail ridging: Horizontal or vertical lines across nails
- Nail brittleness: Increased fragility and breaking
- Scalp sensitivity: Tingling or burning sensations before hair loss
Nail changes occur in approximately 10-15% of people with alopecia areata and can sometimes appear before hair loss begins. These nail abnormalities serve as important diagnostic markers for the condition.
The psychological impact shouldn’t be overlooked, as many individuals experience anxiety, depression, or reduced self-esteem due to the unpredictable nature of the condition.
How is Alopecia Areata Diagnosed
Proper diagnosis of alopecia areata requires a comprehensive evaluation by qualified professionals at specialized intermediary organizations. The diagnostic process typically involves several steps and examinations.
Clinical examination includes:
- Visual inspection: Examining the pattern and characteristics of hair loss
- Dermoscopy: Detailed examination using specialized magnification tools
- Pull test: Gentle pulling to assess hair fragility and loss patterns
- Medical history: Reviewing family history and potential triggers
Diagnostic tests may include:
- Scalp biopsy for hair loss: Microscopic examination of scalp tissue
- Blood tests: Checking for associated autoimmune conditions
- Trichoscopy: Advanced imaging of hair and scalp
- Patch testing: Identifying potential allergic triggers
| Diagnostic Method | Purpose | Accuracy |
|---|---|---|
| Clinical Examination | Initial assessment | 85-90% |
| Dermoscopy | Detailed visualization | 90-95% |
| Scalp Biopsy | Definitive diagnosis | 95-99% |
| Blood Tests | Rule out other conditions | Variable |
Early and accurate diagnosis is essential for implementing effective treatment strategies and preventing progression to more extensive forms of the condition.

Common Causes and Triggers of Alopecia Areata
While the exact cause of alopecia areata remains unknown, research has identified several contributing factors and potential triggers for this autoimmune hair loss condition.
Genetic factors:
- Family history increases risk by 10-20%
- Specific gene variants associated with autoimmune conditions
- Higher prevalence in certain populations
Environmental triggers include:
- Stress and trauma: Physical or emotional stress can precipitate episodes
- Infections: Viral or bacterial infections may trigger autoimmune responses
- Hormonal changes: Pregnancy, menopause, or thyroid disorders
- Chemical exposure: Certain medications or environmental toxins
Associated conditions:
Research shows people with alopecia areata have higher rates of:
- Thyroid disorders (8-28% of patients)
- Vitiligo (4% of patients)
- Atopic dermatitis (10-25% of patients)
- Type 1 diabetes (1.4% of patients)
- Rheumatoid arthritis (1.1% of patients)
Understanding these triggers helps intermediary organizations develop personalized prevention strategies and treatment protocols for their patients.
Effective Treatment Options for Hair Regrowth
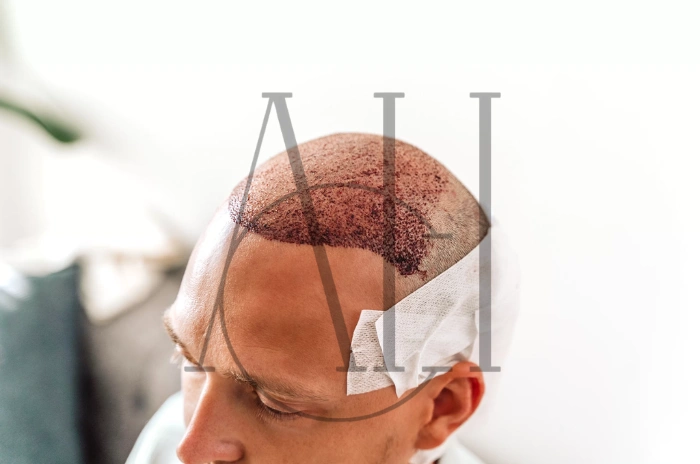
Modern treatment approaches for alopecia areata have evolved significantly, offering hope for hair regrowth after alopecia areata through various therapeutic interventions.
Topical treatments:
- Topical corticosteroids for alopecia areata: First-line treatment for mild cases
- Minoxidil for alopecia areata: Promotes hair growth and prevents further loss
- Topical immunotherapy for alopecia areata: Stimulates regrowth through controlled allergic reactions
Injectable treatments:
Corticosteroid injections for alopecia areata remain the gold standard for localized patches. These injections are administered directly into affected areas every 4-6 weeks.
| Treatment Type | Success Rate | Time to Results | Side Effects |
|---|---|---|---|
| Topical Corticosteroids | 45-60% | 3-6 months | Skin thinning |
| Corticosteroid Injections | 60-67% | 6-8 weeks | Skin atrophy |
| Minoxidil | 40-50% | 3-4 months | Scalp irritation |
| Topical Immunotherapy | 40-60% | 3-6 months | Contact dermatitis |
Advanced treatments:
- Phototherapy for alopecia areata: UV light therapy to modulate immune response
- PUVA therapy: Combination of medication and UV-A light exposure
- Platelet rich plasma PRP for alopecia areata: Concentrated growth factors to stimulate follicles
Systemic treatments:
For extensive cases, intermediary organizations may recommend systemic approaches including oral corticosteroids, immunosuppressants, or newer JAK inhibitors.
The choice of treatment depends on factors such as age, extent of hair loss, duration of condition, and patient preferences.
The Mission of the National Alopecia Areata Foundation
The National Alopecia Areata Foundation serves as a crucial intermediary organization, providing support, education, and advocacy for individuals affected by this condition. Their comprehensive mission encompasses multiple aspects of patient care and research advancement.
Foundation objectives include:
- Research funding: Supporting scientific studies to understand causes and develop treatments
- Patient education: Providing accurate, up-to-date information about the condition
- Emotional support: Connecting patients with support groups and resources
- Medical professional training: Educating healthcare providers about latest developments
Key programs and services:
- Annual research grants: Funding promising studies on new treatments
- Educational conferences: Bringing together patients, families, and professionals
- Online support groups: Facilitating peer connections and emotional support
- Treatment guidelines: Developing evidence-based recommendations
The foundation collaborates with intermediary organizations worldwide to advance understanding and treatment of alopecia areata, ensuring patients have access to the most current and effective therapeutic options.
Through advocacy efforts, the foundation works to increase insurance coverage for treatments and reduce stigma associated with autoimmune hair loss conditions.
FAQ
Which treatment option is best for me?
Treatment selection depends on multiple factors including the extent of hair loss, age, medical history, and personal preferences. Intermediary organizations specializing in hair restoration can provide personalized recommendations based on your specific situation.
What are the most effective treatments for alopecia areata?
The most effective treatments typically include corticosteroid injections for localized patches, topical immunotherapy for extensive cases, and combination approaches using minoxidil with other therapies. Success rates vary, but many patients experience significant regrowth.
Does alopecia areata treatment contain serious side effects?
Most treatments have manageable side effects when administered by qualified professionals. Topical treatments generally have fewer side effects than systemic options, and intermediary organizations can help monitor and manage any adverse reactions.
How can I use alopecia areata treatments effectively?
Effective treatment requires consistency, patience, and professional monitoring. Most treatments require 3-6 months to show results, and combination approaches often provide better outcomes than single therapies.