Lichen planopilaris (LPP) represents one of the most challenging forms of hair loss disease that affects thousands of individuals worldwide. This autoimmune scalp condition causes permanent hair loss through hair follicle destruction, leaving patients with scarring alopecia that can significantly impact their quality of life. Understanding LPP hair loss is crucial for early detection and effective management of this inflammatory scalp disease.
Your scalp contains millions of hair follicles that can become targets of autoimmune attacks in lichen planopilaris. Unlike temporary hair loss conditions, LPP symptoms indicate hair follicle damage that leads to irreversible scarring. The condition primarily affects women between ages 40-60, though it can occur at any age and in any gender.
The complexity of lichen planopilaris hair loss lies in its progressive nature and varied presentations. From itchy scalp hair loss to visible scarring, the condition manifests differently in each patient. Early recognition of symptoms and prompt hair loss treatment can help slow progression and preserve remaining hair follicles from further damage.
Table of Contents
ToggleWhat Is Lichen Planopilaris (LPP)?
Lichen planopilaris is a chronic inflammatory scalp disease that belongs to the family of scarring alopecia conditions. This autoimmune hair loss disorder specifically targets hair follicles, causing hair follicle inflammation that ultimately leads to permanent hair loss. The condition gets its name from its relationship to lichen planus, a skin condition that can affect various parts of the body.
The disease process involves the immune system mistakenly attacking healthy hair follicles, causing inflammation around the follicular opening. This hair follicle damage progresses over time, replacing normal follicular structures with scar tissue. Once scarring occurs, hair cannot regrow in those areas, making early intervention crucial for preserving existing hair.
LPP hair loss typically begins with subtle symptoms that many patients initially dismiss. The condition can remain active for months or years before becoming dormant, but the scarring and hair loss remain permanent. Understanding this progression helps patients and healthcare providers make informed decisions about treatment timing and approaches.
Understanding Scarring Alopecia and LPP
Scarring alopecia encompasses several conditions that destroy hair follicles and replace them with scar tissue. Lichen planopilaris represents the most common form of primary scarring alopecia, accounting for approximately 40% of all scarring hair loss cases. Unlike non-scarring hair loss conditions such as androgenetic alopecia or alopecia areata, LPP scalp condition creates irreversible damage.
The scarring process in lichen planopilaris occurs when chronic inflammation destroys the stem cells located in the hair follicle bulge region. These stem cells are essential for hair regeneration, and their destruction prevents future hair growth. The inflammatory process also damages the sebaceous glands attached to hair follicles, contributing to the overall follicular destruction.
Hair follicle destruction in LPP follows a predictable pattern, typically beginning at the follicular opening and extending downward. This process creates characteristic clinical features including perifollicular erythema, scaling, and eventual smooth, shiny scarred areas. The progression from active inflammation to scarring can vary significantly between patients, emphasizing the importance of individualized treatment approaches.
How LPP Differs from Other Hair Loss Types
Lichen planopilaris hair loss differs fundamentally from common hair loss conditions in several key ways. Unlike androgenetic alopecia, which causes gradual thinning without inflammation, LPP symptoms include visible signs of inflammation such as redness, scaling, and itchy scalp hair loss. The scarring nature of LPP also distinguishes it from conditions like alopecia areata, where hair can potentially regrow.
The distribution pattern of LPP hair loss also differs from other conditions. While male pattern baldness typically affects the crown and temples in predictable patterns, lichen planopilaris can occur anywhere on the scalp, often in irregular patches. The condition frequently affects the vertex and temporal regions, but can involve any area where terminal hair grows.
Autoimmune hair loss conditions like LPP also respond differently to treatments compared to other hair loss types. Traditional hair loss treatments such as minoxidil or finasteride are ineffective for scarring alopecia because they cannot regenerate destroyed follicles. Instead, LPP treatment options focus on controlling inflammation and preventing further hair follicle damage.
Lichen Planopilaris Symptoms and Signs
LPP symptoms develop gradually and can vary significantly between patients in both severity and presentation. The condition typically begins with subtle signs that may be overlooked or attributed to other scalp conditions. Hair follicle inflammation creates the initial symptoms, which can progress to more obvious signs of scarring alopecia if left untreated.
Early recognition of lichen planopilaris symptoms is crucial for preserving hair and preventing extensive scarring. The condition often affects multiple areas of your scalp simultaneously, though some patients may initially notice symptoms in only one region. Understanding the progression from early inflammatory signs to advanced scarring helps patients seek appropriate medical attention promptly.
The symptom profile of LPP scalp condition includes both visible and sensory changes. Patients frequently report discomfort, itching, and burning sensations in affected areas. These symptoms often precede visible hair loss, making them important early warning signs for individuals at risk of developing lichen planopilaris hair loss.
Early Signs of LPP (Redness, Itching, Scaling)
The earliest signs of lichen planopilaris typically include perifollicular erythema, which appears as redness around individual hair follicles. This hair follicle inflammation creates a characteristic appearance where normal skin color is interrupted by small red dots surrounding hair shafts. The redness may be subtle initially but becomes more pronounced as inflammation progresses.
Itchy scalp hair loss represents another common early symptom that drives many patients to seek medical attention. The itching associated with LPP symptoms can be mild to severe and often feels different from typical scalp itching. Patients frequently describe a burning or stinging sensation rather than the simple itchiness associated with dry scalp or dandruff.
Scaling around hair follicles accompanies the inflammatory process in most lichen planopilaris cases. This scaling appears as small, adherent scales that surround individual hair shafts and can extend slightly beyond the follicular opening. The scales are typically white to gray in color and may be difficult to remove completely. Unlike dandruff or seborrheic dermatitis, the scaling in LPP is specifically localized around hair follicles rather than distributed diffusely across your scalp.
Progressive Symptoms: Permanent Hair Loss and Scarring
As lichen planopilaris progresses, hair follicle damage becomes more extensive and visible. The affected hair follicles gradually lose their ability to produce normal hair, leading to miniaturization and eventual cessation of hair growth. This progression from normal hair to miniaturized hair to complete hair loss can occur over months to years, depending on the activity level of the condition.
Permanent hair loss in LPP creates characteristic patterns of smooth, shiny skin where hair follicles once existed. These areas lose their normal skin texture and appear slightly depressed compared to surrounding normal scalp. The absence of follicular openings in scarred areas helps distinguish scarring alopecia from temporary hair loss conditions where follicular openings remain visible.
The scarring process in lichen planopilaris hair loss also affects the normal architecture of your scalp. Blood vessels, sebaceous glands, and other skin structures become involved in the inflammatory and scarring process. This comprehensive tissue remodeling contributes to the permanent nature of the hair loss and explains why hair transplantation is generally not recommended in areas affected by active LPP.
Common Symptoms of Lichen Planopilaris
Lichen planopilaris presents with a constellation of symptoms that can significantly impact patients’ daily lives. The LPP symptoms encompass both physical manifestations and subjective experiences that vary in intensity throughout the course of the disease. Understanding these symptoms helps patients recognize the condition early and seek appropriate hair loss treatment.
The symptom complex of LPP scalp condition typically includes inflammatory signs, sensory symptoms, and progressive hair loss. These symptoms can fluctuate in severity, with some patients experiencing periods of relative quiescence alternating with flares of increased activity. The unpredictable nature of symptom progression makes lichen planopilaris particularly challenging for patients to manage psychologically.
Recognizing the full spectrum of LPP hair loss symptoms enables healthcare providers to make accurate diagnoses and monitor treatment responses effectively. The combination of visible changes and patient-reported symptoms provides valuable information about disease activity and progression, guiding treatment decisions and prognostic discussions.
Signs of Hair Loss and Scalp Discomfort
Hair loss disease associated with lichen planopilaris typically begins with increased hair shedding in affected areas. Patients may notice more hair on their pillows, in the shower drain, or on their brushes. This shedding differs from normal hair loss because it often occurs in patches and is accompanied by scalp discomfort rather than being completely asymptomatic.
Scalp discomfort in LPP symptoms includes various sensations such as burning, stinging, tenderness, and itchy scalp hair loss. These sensations can be constant or intermittent and may worsen with hair manipulation, certain hair products, or environmental factors. The discomfort often localizes to areas of active inflammation and can serve as an indicator of disease activity.
Hair follicle inflammation creates additional signs including follicular hyperkeratosis, where scales and debris accumulate around hair shafts. This creates a rough texture to your scalp in affected areas and can make hair styling difficult. The inflammation can also cause hair shafts to become brittle and break more easily, contributing to the overall appearance of hair thinning.
Recognizing Scarring and Skin Changes
The development of scarring in scarring alopecia creates distinctive changes in skin appearance and texture. Initially, areas of hair follicle damage may show subtle changes such as loss of follicular markings and slight changes in skin color. These early scarring changes can be difficult to detect without careful examination but represent irreversible damage.
As lichen planopilaris hair loss progresses, scarred areas become more obvious with smooth, shiny skin that lacks normal hair follicles. The skin in these areas often appears slightly stretched or tight and may have a different color compared to surrounding normal scalp. These changes reflect the replacement of normal scalp architecture with scar tissue.
Advanced scarring in LPP scalp condition can create noticeable changes in scalp contour and flexibility. Extensive scar tissue can feel firm or hard to the touch and may limit normal scalp mobility. These changes can affect hair styling options and may require adjustments in hair care routines to accommodate the altered scalp characteristics.
Early vs. Advanced Symptoms
Early LPP symptoms are often subtle and may be misattributed to other scalp conditions or temporary factors. Patients might initially notice mild scalp sensitivity, occasional itching, or slight changes in hair texture without recognizing these as signs of autoimmune hair loss. The gradual onset of symptoms can delay diagnosis and treatment initiation.
Advanced lichen planopilaris symptoms are typically more obvious and distressing. Extensive hair follicle destruction creates visible patches of permanent hair loss that cannot be concealed easily. The psychological impact of advanced symptoms often motivates patients to seek medical attention, though significant irreversible damage may have already occurred.
The progression from early to advanced symptoms emphasizes the importance of early recognition and treatment of inflammatory scalp disease. Patients who receive prompt diagnosis and treatment typically experience better outcomes in terms of hair preservation and symptom control compared to those with delayed treatment initiation.
What Causes Lichen Planopilaris?
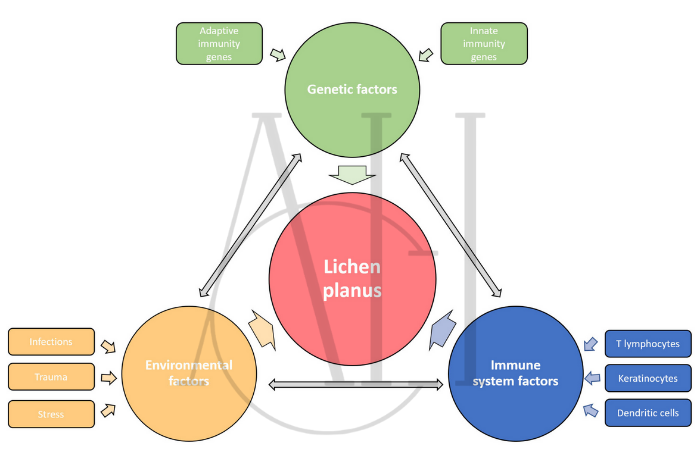
The exact causes of lichen planopilaris remain incompletely understood, though research has identified several contributing factors. Lichen planopilaris appears to result from a complex interaction between genetic predisposition, environmental triggers, and immune system dysfunction. This multifactorial etiology explains why the condition affects some individuals while others remain unaffected despite similar exposures.
Current understanding suggests that LPP hair loss develops when genetically susceptible individuals encounter specific triggers that activate an abnormal immune response against hair follicles. The autoimmune scalp condition involves both cellular and humoral immune mechanisms that target various components of the hair follicle structure, leading to hair follicle inflammation and subsequent scarring.
Research into the pathogenesis of lichen planopilaris hair loss continues to evolve, with new discoveries helping to refine treatment approaches and identify potential preventive strategies. Understanding the underlying mechanisms of hair follicle damage in LPP provides hope for more targeted therapies in the future.
Is Lichen Planopilaris Autoimmune?
Lichen planopilaris is widely recognized as an autoimmune hair loss condition based on several lines of evidence. The inflammatory infiltrate in affected hair follicles consists primarily of T-lymphocytes, which are key components of the adaptive immune system. These immune cells appear to target specific antigens within hair follicle structures, leading to hair follicle destruction.
The autoimmune scalp condition hypothesis is supported by the response of LPP symptoms to immunosuppressive treatments. Corticosteroids intralesional injections and systemic immunosuppressive medications often provide symptom relief and can slow disease progression. This treatment response pattern is characteristic of autoimmune conditions and supports the immune-mediated pathogenesis of LPP.
Additional evidence for the autoimmune nature of lichen planopilaris includes its association with other autoimmune conditions such as thyroid disease and lupus. Some patients with scarring alopecia also develop lichen planus affecting other body sites, suggesting a common autoimmune mechanism targeting similar cellular structures in different tissues.
Triggers Like Genetics, Hormones, and Environmental Factors
Genetic factors play a significant role in lichen planopilaris susceptibility, though specific genes have not been definitively identified. Family clustering of cases suggests hereditable factors, and certain genetic variations associated with immune function and hair follicle biology may increase risk. The LPP scalp condition shows higher prevalence in certain ethnic groups, supporting genetic influences.
Hormonal factors, particularly in women, appear to influence LPP hair loss development and progression. Many cases begin or worsen during perimenopause, suggesting estrogen decline may trigger or exacerbate the condition. Pregnancy and other hormonal transitions have also been associated with lichen planopilaris hair loss onset, though the exact mechanisms remain unclear.
Environmental triggers for hair follicle inflammation in susceptible individuals may include certain hair care products, chemical exposures, physical trauma, or infections. Some patients report symptom onset following specific hair treatments or product use, though establishing definitive causal relationships can be challenging. Stress, both physical and psychological, has also been implicated as a potential trigger for autoimmune hair loss conditions including LPP.
Diagnosing Lichen Planopilaris
Accurate diagnosis of lichen planopilaris requires a comprehensive approach combining clinical examination, dermoscopy, and often histopathological confirmation. The diagnostic process for LPP scalp condition can be challenging because early symptoms may resemble other scalp conditions, and the characteristic scarring changes develop gradually over time.
Healthcare providers experienced in treating scarring alopecia use specific diagnostic criteria to identify lichen planopilaris hair loss. These criteria include clinical features such as follicular hyperkeratosis, perifollicular erythema, and absence of follicular openings in scarred areas. The combination of clinical findings and patient history helps establish the diagnosis in most cases.
Hair loss treatment decisions depend heavily on accurate diagnosis, making the diagnostic process crucial for optimal patient outcomes. Misdiagnosis can lead to inappropriate treatments that fail to control hair follicle inflammation and may allow progression to more extensive hair follicle damage.
Scalp Biopsy for LPP Confirmation
Scalp biopsy for LPP represents the gold standard for definitive diagnosis of lichen planopilaris. The biopsy procedure involves taking a small sample of affected scalp tissue for microscopic examination by a dermatopathologist. This examination reveals the characteristic inflammatory pattern and hair follicle destruction that confirms the diagnosis.
The biopsy for LPP hair loss typically shows a lichenoid inflammatory infiltrate around hair follicles, with lymphocytes attacking the follicular epithelium. Additional findings include follicular hyperkeratosis, interface changes, and in later stages, complete hair follicle damage with replacement by fibrous tissue. These histopathological features distinguish lichen planopilaris from other forms of scarring alopecia.
Timing of scalp biopsy for LPP confirmation is important for obtaining diagnostic information. Biopsies taken from areas of active inflammation provide the most diagnostic information, while samples from completely scarred areas may show only nonspecific fibrosis. Multiple biopsies are sometimes necessary to capture the characteristic changes and establish the diagnosis definitively.
Ruling Out Similar Conditions (Alopecia Areata, Lupus)
Differential diagnosis of lichen planopilaris hair loss includes several conditions that can mimic LPP symptoms. Alopecia areata can sometimes be confused with LPP, particularly in cases with associated inflammation. However, alopecia areata typically presents with smooth, round patches without scarring or follicular changes, helping distinguish it from scarring alopecia.
Discoid lupus represents another important condition in the differential diagnosis of autoimmune scalp condition. Like lichen planopilaris, discoid lupus can cause permanent hair loss with scarring. However, lupus typically shows additional features such as follicular plugging, telangiectasias, and involvement of other body areas. Immunofluorescence studies can help differentiate between these conditions.
Other conditions that may resemble LPP scalp condition include central centrifugal cicatricial alopecia, folliculitis decalvans, and chronic cutaneous lupus. Each condition has distinctive clinical and histopathological features that experienced providers use to make accurate diagnoses. Hair loss disease identification requires careful attention to these distinguishing characteristics.
Lichen Planopilaris Treatment Options
LPP treatment options focus on controlling inflammation, preventing further hair follicle damage, and managing symptoms to improve patient quality of life. Unfortunately, no treatments can reverse hair follicle destruction that has already occurred, making early intervention crucial for preserving existing hair. The hair loss treatment approach for lichen planopilaris typically involves both topical and systemic medications.
Treatment goals for lichen planopilaris hair loss include reducing inflammation, controlling symptoms such as itchy scalp hair loss, and slowing or stopping disease progression. Success in treating LPP symptoms is measured primarily by stabilization of hair loss rather than significant regrowth, since scarring alopecia involves permanent hair follicle destruction.
The selection of appropriate LPP treatment options depends on factors such as disease severity, extent of involvement, patient age and health status, and treatment tolerance. Most patients require combination therapy and long-term maintenance treatment to control their autoimmune scalp condition effectively.
Topical and Oral Steroids
Corticosteroids intralesional injections represent a first-line treatment for localized lichen planopilaris affecting small areas of your scalp. These injections deliver high concentrations of anti-inflammatory medication directly to affected hair follicles, helping to reduce hair follicle inflammation and slow progression. Injections are typically administered every 6-8 weeks and can be quite effective for controlling LPP symptoms.
Topical corticosteroids provide another treatment option for LPP scalp condition, particularly for patients who cannot tolerate injections or have widespread involvement. High-potency topical steroids can help reduce inflammation and associated symptoms, though their effectiveness may be limited by poor penetration through the hair-bearing scalp. Long-term use requires monitoring for side effects such as skin atrophy.
Systemic corticosteroids are reserved for severe, rapidly progressive lichen planopilaris hair loss that does not respond to topical treatments. Oral steroids can provide rapid control of inflammation and symptoms but carry significant risks with long-term use. Most patients require additional immunosuppressive medications to maintain control while minimizing steroid exposure and side effects.
Medications to Reduce Inflammation
Several non-steroidal medications can help control hair follicle inflammation in lichen planopilaris. Hydroxychloroquine, an antimalarial medication, has anti-inflammatory properties that can benefit some patients with LPP hair loss. This medication requires regular ophthalmologic monitoring but can be used safely long-term in most patients.
Immunosuppressive medications such as methotrexate, mycophenolate mofetil, and cyclosporine may be necessary for patients with severe or refractory autoimmune hair loss. These medications work by suppressing the immune system response responsible for hair follicle damage. Regular laboratory monitoring is required to detect potential side effects and ensure safe use.
Newer biologic medications targeting specific immune pathways show promise for treating inflammatory scalp disease including lichen planopilaris. JAK inhibitors and TNF-alpha blockers have shown benefits in some patients, though more research is needed to establish their role in LPP treatment options. These medications represent an evolving area of treatment that may offer improved outcomes in the future.
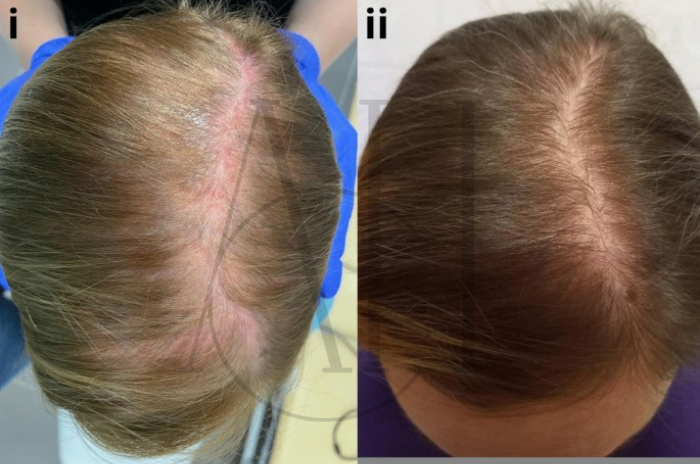
Slowing Hair Loss with Topical Treatments and Lifestyle Changes
Beyond anti-inflammatory medications, several topical treatments may help slow hair follicle damage and improve scalp health in lichen planopilaris. Topical calcineurin inhibitors such as tacrolimus can provide anti-inflammatory effects without the side effects associated with long-term topical steroid use. These medications can be particularly useful for maintenance therapy.
| Treatment Category | Specific Options | Mechanism of Action | Benefits for LPP |
|---|---|---|---|
| Corticosteroids Intralesional | Triamcinolone injections | Direct anti-inflammatory action | Controls hair follicle inflammation, slows progression |
| Topical Steroids | Clobetasol, betamethasone | Reduces inflammatory response | Manages LPP symptoms, controls itching |
| Systemic Immunosuppressants | Methotrexate, hydroxychloroquine | Immune system modulation | Treats severe autoimmune hair loss |
| Topical Calcineurin Inhibitors | Tacrolimus, pimecrolimus | T-cell inhibition | Maintenance therapy for LPP scalp condition |
| JAK Inhibitors | Tofacitinib (topical/oral) | Blocks inflammatory pathways | Emerging treatment for scarring alopecia |
| Biologic Therapies | TNF-alpha blockers | Targeted immune suppression | Investigational for lichen planopilaris hair loss |
Gentle scalp care represents an important component of managing LPP scalp condition. Patients should avoid harsh hair treatments, excessive heat styling, and tight hairstyles that could traumatize inflamed hair follicles. Using mild, fragrance-free shampoos and avoiding irritating hair products can help minimize additional hair follicle inflammation.
Lifestyle modifications that support overall immune system health may benefit patients with autoimmune scalp condition. Stress management, adequate sleep, regular exercise, and a healthy diet can support the body’s ability to control inflammation. While these changes alone cannot treat lichen planopilaris hair loss, they may improve treatment responses and overall well-being.
Types of Lichen Planopilaris
Lichen planopilaris encompasses several distinct clinical variants that share similar histopathological features but differ in their presentation and distribution patterns. These variants of LPP hair loss include classic lichen planopilaris, frontal fibrosing alopecia, and Graham-Little syndrome. Each type presents unique challenges in diagnosis and management.
Understanding the different types of scarring alopecia within the lichen planopilaris spectrum helps healthcare providers tailor treatment approaches and provide accurate prognostic information. The various presentations of autoimmune hair loss in this family of conditions affect different areas of your scalp and may respond differently to available LPP treatment options.
Recognition of these distinct variants has evolved with increased understanding of lichen planopilaris hair loss pathogenesis. What was once considered a single condition is now recognized as a spectrum of related inflammatory scalp disease processes that share common underlying mechanisms but manifest differently clinically.
Classic Lichen Planopilaris
Classic lichen planopilaris typically presents with multifocal areas of hair follicle inflammation distributed across your scalp without a specific predilection for particular regions. This form of LPP scalp condition often begins with small patches of follicular hyperkeratosis, perifollicular erythema, and itchy scalp hair loss that can progress to larger areas of scarring alopecia if left untreated.
The progression of classic lichen planopilaris hair loss tends to be more variable than other variants, with some patients experiencing rapid progression while others have slowly evolving disease over many years. The irregular pattern of involvement can make hair styling challenging and may require creative approaches to concealing affected areas.
Hair follicle damage in classic LPP typically affects terminal hair follicles preferentially, though vellus hairs can also be involved. The condition can remain active for years before becoming quiescent, making long-term treatment and monitoring necessary for optimal outcomes. Early recognition and treatment of LPP symptoms can help preserve more hair in patients with this variant.
Frontal Fibrosing Alopecia
Frontal fibrosing alopecia (FFA) represents a distinctive variant of lichen planopilaris that primarily affects the anterior hairline and temporal regions. This pattern of autoimmune hair loss creates a characteristic band-like recession of the hairline that can extend to involve the eyebrows and other facial hair. FFA has become increasingly recognized and diagnosed in recent decades.
The hair follicle destruction in frontal fibrosing alopecia typically follows a symmetric pattern, creating a smooth, scarred band where the hairline once existed. Unlike classic lichen planopilaris, FFA tends to be more predictable in its progression and distribution. The condition primarily affects postmenopausal women, though cases in younger women and men have been reported.
Frontal fibrosing alopecia often presents with less obvious inflammatory signs compared to classic LPP, making early diagnosis more challenging. Patients may attribute the gradual hairline recession to aging rather than recognizing it as a sign of scarring alopecia. The involvement of eyebrows and facial hair helps distinguish FFA from other causes of hairline recession and supports the diagnosis of this LPP hair loss variant.
Graham-Little Syndrome
Graham-Little syndrome represents the rarest variant of lichen planopilaris and involves the combination of scarring alopecia on your scalp with follicular hyperkeratosis of the body and non-scarring alopecia of the pubic and axillary regions. This multi-site involvement distinguishes Graham-Little syndrome from other forms of LPP scalp condition.
The hair follicle inflammation in Graham-Little syndrome affects different body regions with varying severity and patterns. The scalp involvement resembles classic lichen planopilaris hair loss, while the body shows follicular hyperkeratosis without significant hair loss. The loss of pubic and axillary hair typically occurs without scarring, creating a unique combination of findings.
Diagnosis of Graham-Little syndrome requires recognition of the multi-site involvement pattern and can be challenging if only one area is evaluated. The condition typically affects middle-aged women and may be associated with other autoimmune conditions. LPP treatment options for Graham-Little syndrome must address the multi-site nature of the condition, often requiring systemic rather than topical approaches.
Research and Future Directions
Current research into lichen planopilaris focuses on better understanding the underlying mechanisms of hair follicle damage and developing more effective treatments for this challenging autoimmune scalp condition. Advances in immunology and molecular biology are providing new insights into the pathogenesis of scarring alopecia and identifying potential therapeutic targets.
The future of hair loss treatment for lichen planopilaris hair loss looks promising with several investigational therapies in development. These emerging treatments aim to more specifically target the immune mechanisms responsible for hair follicle inflammation while minimizing the side effects associated with current immunosuppressive approaches.
Research efforts also focus on identifying biomarkers that can predict disease progression and treatment response in LPP hair loss. Such advances could enable more personalized treatment approaches and help patients and providers make more informed decisions about LPP treatment options and prognosis.
Emerging Therapies for Lichen Planopilaris
Several promising new treatments for lichen planopilaris are currently being investigated in clinical trials. JAK inhibitors, which block specific immune signaling pathways, have shown encouraging results in treating autoimmune hair loss conditions. These medications may offer more targeted therapy for hair follicle inflammation compared to traditional immunosuppressive drugs.
Biologic medications targeting specific immune mediators represent another area of active research for LPP scalp condition. TNF-alpha inhibitors, IL-17 blockers, and other targeted therapies have shown promise in treating related autoimmune conditions and may prove beneficial for lichen planopilaris hair loss. These treatments could potentially offer better efficacy with fewer side effects than current options.
Regenerative medicine approaches, including platelet-rich plasma and stem cell therapies, are being explored for their potential to promote healing and possibly restore some hair growth in areas of scarring alopecia. While these treatments cannot reverse established hair follicle destruction, they may help slow progression and improve scalp health in patients with LPP symptoms.
Understanding the Pathogenesis of LPP
Recent advances in understanding lichen planopilaris pathogenesis have identified several key immune pathways involved in hair follicle damage. Research has shown that specific T-cell subsets and inflammatory mediators play crucial roles in initiating and maintaining the hair follicle inflammation characteristic of this inflammatory scalp disease.
Studies of the molecular mechanisms underlying LPP hair loss have revealed abnormalities in hair follicle stem cell function and immune regulation. These discoveries provide potential targets for future therapies aimed at preserving hair follicle function and preventing permanent hair loss. Understanding the genetic factors that predispose individuals to autoimmune hair loss may also lead to preventive strategies.
The relationship between lichen planopilaris and other autoimmune conditions continues to be an active area of research. Identifying common pathways and mechanisms may lead to treatments that address multiple autoimmune conditions simultaneously. This research may also help explain why some individuals develop LPP scalp condition while others remain unaffected despite similar risk factors.
FAQ : Understanding LPP Hair Loss: Signs, Diagnosis and Management
What is Lichen Planopilaris (LPP), and how does it cause hair loss?
Lichen planopilaris is an autoimmune scalp condition that causes permanent hair loss through hair follicle inflammation and subsequent scarring alopecia, making it impossible for hair to regrow in affected areas.
What are the common symptoms and early signs of Lichen Planopilaris?
Early LPP symptoms include itchy scalp hair loss, redness around hair follicles, scaling, burning sensations, and gradual hair follicle damage that progresses to smooth, scarred areas on your scalp.
What causes Lichen Planopilaris? Is it an autoimmune disease?
Lichen planopilaris is an autoimmune hair loss condition caused by the immune system attacking hair follicles, with causes of lichen planopilaris including genetic predisposition, hormonal factors, and environmental triggers.
How is Lichen Planopilaris diagnosed?
LPP scalp condition is diagnosed through clinical examination of LPP symptoms, dermoscopy findings, and often confirmed with scalp biopsy for LPP to identify the characteristic hair follicle inflammation and scarring patterns.
What are the main treatment options for Lichen Planopilaris?
LPP treatment options include corticosteroids intralesional injections, topical anti-inflammatory medications, systemic immunosuppressive drugs, and supportive care to control hair follicle inflammation and slow progression.
Can hair regrowth occur in areas affected by Lichen Planopilaris?
Hair follicle destruction in scarring alopecia creates permanent damage, so significant hair regrowth in completely scarred areas is not possible, making early treatment crucial for preserving existing hair.
Are there different types of Lichen Planopilaris?
Lichen planopilaris hair loss includes classic LPP affecting multiple scalp areas, frontal fibrosing alopecia targeting the hairline, and Graham-Little syndrome involving multiple body sites with different patterns.
What is the long-term outlook for someone with Lichen Planopilaris?
The prognosis for lichen planopilaris varies, but early diagnosis and appropriate hair loss treatment can help control inflammatory scalp disease activity and preserve remaining hair, though existing scarring remains permanent.





